2025 has, indisputably, been a year of change in oncology as the field grapples with shifting policy directions, RIFs, and uncertainty stemming from the Trump administration’s MAHA mission.


Since 2019, we have been mining The Cancer Letter’s analytics to catch a glimpse of what’s capturing you and your colleagues’ attention each year. In 2025, it’s no question that health care policy has taken center stage.
The Cancer Letter has covered the politics and policy surrounding cancer research since 1973, and a year like 2025 has demanded an expansion of this coverage. We launched Cancer Policy, a new section dedicated to the topic, and many of these articles appeared among our most-read articles.
We also launched a podcast to help make sense of our world as it kept shifting around us. Through this platform, we explored the latest headlines, talked to oncology leaders about the impacts of the latest policy changes, and ran exclusive interviews with cancer center leaders about what’s keeping them up at night.
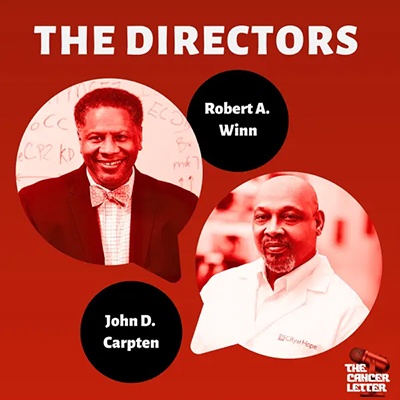
The top episode of the year, The Directors: Rob Winn and John Carpten on the future of cancer centers, kicked off a monthly series of interviews between two cancer center directors, which has featured perspectives from cancer centers across the country—some optimistic, some realistic, and all strategic—sharing the same mission of maintaining stability of the U.S. cancer program.
According to Spotify Wrapped, The Cancer Letter Podcast was a 2025 Marathon Show, Instant Hit Show, and Most Shared Show.
A list of The Cancer Letter’s top stories, grouped by topic, follows:
Top news features
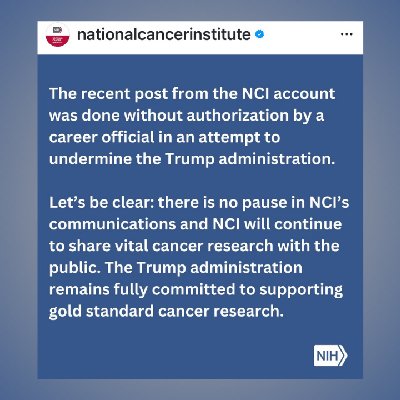
A farewell post by an unidentified NCI employee triggers an accusation of “undermining the Trump administration”
May 30, 2025
In the morning of May 28, presumably before turning off the lights and closing the office door, someone at the now defunct NCI Office of Communications and Public Liaison decided to post a farewell message to the cancer community.
The message, posted on multiple social media accounts, read:
We’re taking a pause here – but not on the mission.
Thanks for being a part of our community. While we won’t be actively posting, you can still find trusted cancer updates via @NIH as NCI’s work continues every day.
The story doesn’t end here.
NIH eliminates the NCI Board of Scientific Advisors
Over its 28 year history, BSA shaped NCI-funded extramural science
May 2, 2025
After nearly three decades of reviewing NCI-funded extramural projects and sometimes saving NCI from its own folly, the Board of Scientific Advisors has been terminated as part of the Trump administration’s drive to reduce the size of the federal government.
Unlike the National Cancer Advisory Board, which is based on a provision of the National Cancer Act of 1971, the 28-member BSA can be dissolved without an act of Congress.
The dissolution of the BSA comes at a time when the government-funded science—including cancer research—is facing an existential threat, which entails a potential 40% cut in appropriations, elimination of NIH institutes and centers, cutting salaries of top officials, and lowering indirect costs to 15%.
One former high-level NCI official said to The Cancer Letter that in the hierarchy of bad things, the elimination of the BSA ranks somewhere around No. 10.
Harold Varmus, a Nobel laureate former NIH and NCI director, largely agreed with this assessment, offering this bit of dark humor:
“If appropriations are slashed, there won’t be any need to evaluate new projects!”
Pediatric cancer research cut from spending legislation at last minute
Republicans quietly removed hard-won pediatric cancer bills
Jan. 10, 2025
On Saturday, Dec. 21, Congress passed a new spending package, narrowly averting a government shutdown.
Approval of the package, however, came at potentially great cost to the pediatric cancer community.
Republicans removed pediatric cancer bills that would have reauthorized the priority review voucher, authorized FDA to direct companies to undertake pediatric cancer novel clinical trials of approved drugs, and ensured that kids on Medicaid could access treatment across state lines.
“I’m just so disappointed that our bills couldn’t stay in the [continuing resolution], because the pediatric cancer community is not a resource-rich community,” Nancy Goodman, founder and executive director of Kids v. Cancer, said to The Cancer Letter.
It’s a community of many bereaved parents, trying to affect change with minimal financial resources, she said.
“We don’t hire professional lobbyists. It’s really a lot of work for us to put these ideas forward,” Goodman said. “I’m just incredibly disappointed that that wasn’t taken into consideration. It’s just an incredible burden for this community to do everything we’re doing in terms of taking care of our kids or missing our kids, and then to try to work with Congress.”
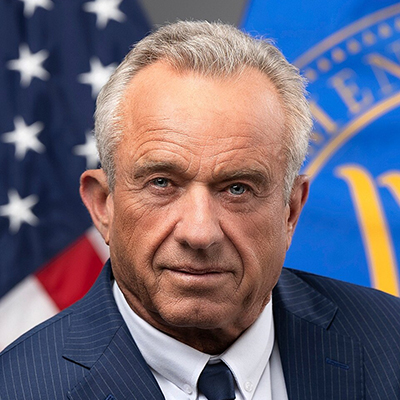
What Trump’s pick of RFK Jr. means for cancer: Epidemics, HPV, stunted research
Former FDA Commissioner Scott Gottlieb expresses “deep concerns”
Dec. 6, 2024
Robert F. Kennedy Jr., an anti-vaccine activist whom Trump has chosen to run HHS, would have the capacity to roll back core public health protections, including protections for people with cancer, and dismantle research related to infectious diseases, public health experts warn.
If he is confirmed by the Senate, Kennedy’s role at HHS would include oversight over CDC, FDA and NIH (The Cancer Letter, Nov. 15, 2024).
“I have deep concerns about Kennedy’s stated intentions to roll back core public health protections, particularly as it relates to childhood vaccines,” Scott Gottlieb, a physician and a former Trump-appointed FDA commissioner, said in an interview aired on CNBC on Nov. 29.
“[Kennedy] has brought in a very experienced team, a lot of lawyers from [Children’s Health Defense], his antivax organization. These people are capable, I think they’re deadly serious, they’ve been very clear about their intentions,” Gottlieb said.
“I think if RFK follows through on his intentions–and I believe he will, and I believe he can–it will cost lives in this country,” Gottlieb said.
Related:
- As Trump’s HHS pick, RFK Jr. stands to honor or squander the Kennedy legacy in cancer (The Cancer Letter, Nov. 15, 2024)
- Don’t confirm RFK Jr. for HHS, 77 Nobel laureates urge the Senate (The Cancer Letter, Dec. 13, 2025)
- With a spotlight on vaccines, abortion, Medicaid and Medicare, RFK Jr. goes before the Senate (The Cancer Letter, Jan. 31, 2025)
- Senate Finance Committee advances RFK Jr. to likely confirmation, with Bill Cassidy (R-LA) casting the deciding vote (The Cancer Letter, Feb. 7, 2025)
- Kennedy announces massive cuts, centralization at HHS—NCI and FDA hit (The Cancer Letter, March 28, 2025)
- RFK Jr. urges FDA staff to resist “agency capture” by special interests and resist “deep state” (The Cancer Letter, April 18, 2025)
- Grilled by Congress, Kennedy defends NIH and NCI budget cuts, freezes, and RIFs (The Cancer Letter, May 16, 2025)
- Kennedy’s claims notwithstanding, NCI clinical trials are delayed, enrollments reduced (The Cancer Letter, May 16, 2025)
- Kennedy: “We’re going to end the war at FDA against alternative medicine” (The Cancer Letter, June 13, 2025)
- At House hearing, Democrats clash with RFK Jr. over “radical obstruction of congressional oversight,” vaccine policies (The Cancer Letter, June 27, 2025)
- With CDC in free fall, RFK Jr. faces bipartisan rebuke at Senate hearing (The Cancer Letter, Sept. 5, 2025)
- After stormy Senate hearing, Trump offers tepid support for RFK Jr. while Kennedy family members call for his ouster (The Cancer Letter, Sept. 12, 2025)
- Science advocates organize march in DC to demand impeachment of RFK Jr. (The Cancer Letter, Oct. 24, 2025)
Rathmell steps down at NCI as Trump team considers candidates to replace her
Wafik El-Deiry, Harvey Risch have been interviewed
Jan. 17, 2025
W. Kimryn Rathmell has stepped down as NCI director, opting to hand her resignation to the Biden administration over facing the uncertainties that Trump and his team are expected to usher in starting next week.
Rathmell’s decision to leave the institute comes after influential members of the cancer community attempted to convince the Trump team to allow her to stay.
The Cancer Letter has confirmed that at least two individuals are being considered—and have been interviewed—for the top job at NCI.
Rathmell’s resignation is effective Jan. 20, the last day of the Biden administration.
Related:
- From January to April, Rathmell wrote a weekly column for The Cancer Letter, “17 and onward”
- Anthony Letai sworn in as 18th NCI director (The Cancer Letter, Oct. 3, 2025)
- Anthony Letai pledges to ensure stability for extramural and intramural cancer science (The Cancer Letter, Dec. 5, 2025)
Beyond the $500B Stargate Project: The frontier of AI in oncology beckons
By Sorena Nadaf-Rahrov, MS, MMI, PhDc, Jan. 24, 2025
On Jan. 21, President Donald Trump announced the launch of the Stargate Project, a $500 billion artificial intelligence infrastructure project designed to revolutionize healthcare.
This groundbreaking privately funded initiative, developed in collaboration with OpenAI, SoftBank, and Oracle, represents one of the most ambitious investments in leveraging AI to advance disease research and treatment development, with a particular focus on “curing cancer.”
Regardless of whether one agrees with its ambitious projections, the Stargate Project has further positioned the United States as a leader in global AI innovation.
However, even with such unprecedented infrastructure investments, the success of the Stargate initiative will ultimately depend on the direct engagement of domain experts across healthcare, particularly in oncology.
GRAIL’s woes raise questions about the prospects of MCDs and standards for their evaluation
Oct. 25, 2024
In an industry that set its sights on reshaping cancer detection, GRAIL Inc. had the appearance of a pioneer.
If any multi-cancer detection test was heading toward FDA approval and broad reimbursement, GRAIL’s Galleri was on track to get there first. Or so it might have seemed—and so the company said.
A large-scale MCD clinical study was underway in the United Kingdom, with 140,000 people receiving the test through the National Health Service. Another study, the Medicare-Galleri study, called REACH, an acronym for Real-world Evidence to Advance Multi-Cancer Early Detection Health Equity, is enrolling 50,000 individuals, allowing for three annual screens.
And GRAIL was in conversations with FDA as far back as 2019 about premarket approval of Galleri. The company publicly projected FDA premarket approval by “mid-2024” and “widespread adoption” by 2025.
Investors were bidding up the stock of Illumina Inc., the company that, like a tango partner, spun off GRAIL, pulled it back in, and ultimately spun it off again. Illumina’s share price peaked at $523 on Aug. 16, 2021.
Even without FDA approval, Galleri was commercially available as a laboratory developed test, and as of June 30, GRAIL had sold more than 215,000 tests. This, as well as the sale of other similar tests, created an imperative for NCI to push for studying the MCDs, even as the institute’s budget continued to stagnate.
The question before NCI was straightforward: Are people tested with MCDs being helped, or are they swallowing sciencey nonsense and getting harmed?
Related:
- Pooled analysis questions reliability of an endpoint used in multi-cancer detection trials (The Cancer Letter, April 12, 2024)
- GRAIL to use new study results to seek FDA approval of Galleri MCD test (The Cancer Letter, Oct. 24, 2025)
- Class action complaint alleging GRAIL insider fraud resubmitted after dismissal (The Cancer Letter, Oct. 31, 2025)
DOD cancer research programs face 57% funding cut in year-long continuing resolution
Pancreatic, lung, kidney cancer research programs eliminated
March 28, 2025
The March 15 continuing resolution has gutted the Department of Defense Congressionally Directed Medical Research Program. The program’s funding was cut by 57%, compared to Fiscal Year 2024 levels—from $1.5 billion to $650 million.
Some cancer research advocates were told that CDMRP would spread out the remaining $650 million proportionally across its 35 FY24 research programs. Instead, CDMPR slashed more than half of its programs. CDMRP will fund only 12 in FY25.
The cancer research programs that have been eliminated are:
- The Lung Cancer Research Program, which was given $25 million in FY24
“We were asking for $60 million for lung cancer research, with solid justification for that relatively modest ask,” Dusty Donaldson, co-chair of the Lung Cancer Action Network, said to The Cancer Letter. “Instead, we were blindsided by the Lung Cancer Research Program being cut from the program, based on the CDMRP announcement that does not include lung cancer funding.
“Lung cancer is the number one cancer killer, hands down. Yet, lung cancer is one of the least funded cancer research programs under CDMRP. We did not see this coming. Not only did we not get the $60 million we were hoping for, apparently, the $25 million that had been in last year’s budget was slashed to zero. Frankly, we are devastated… It will be difficult for us to start at zero—setting us back decades.” - The Pancreatic Cancer Research Program, which was given $15 million in FY24
“These dollars were important to our community,” Julie Fleshman, president and CEO of the Pancreatic Cancer Action Network, said to The Cancer Letter. “What does this say to patients and families and what does this say to our research community when you completely cut it?” Fleshman said. “You think, how can it all be taken away just like that?
“The fact that it’s cut completely is just really devastating. It’s disheartening. I am sad for our researchers who are working so hard to make advances in this disease. And ultimately our patients will suffer because the new progress that would’ve come out of those dollars will not move forward.” - The Kidney Cancer Research Program, which was given $50 million in FY24
“CDMRP isn’t redundant; it’s irreplaceable,” the Kidney Cancer Association said in a statement. “It backs research NIH or other programs may not be able to currently fund. It empowers patient-centered innovation. And it saves lives.”
Related:
Breast cancer activists in the 90s got DOD to fund cancer research—now that program has been gutted (The Cancer Letter, March 28, 2025)
The faces of RIF: Staff members of NCI’s dissolved communications team gather for a farewell group photo
May 23, 2025
On May 21, staff members of NCI’s dissolved Office of Communications and Public Liaison and friends gathered at the house of Peter Garrett and Ken Crerar.
Garrett, who as the director for External Affairs oversaw the institute’s communications, legislative affairs, and advocacy relations, retired on May 9.
In the first week of May, NCI was left incommunicado as NIH eliminated the communications branch (The Cancer Letter, May 9, 2025).
Knight Cancer Institute receives record-setting $2B gift from the Knights—and self-governance within OHSU
Brian Druker returns to executive role as president of the new Knight Cancer Group
Aug. 14, 2025
Phil and Penny Knight made a record-setting $2 billion gift to OHSU Knight Cancer Institute.
The gift—which appears to be the largest single donation ever made to any U.S. university, college or academic health center—was announced together with an organizational restructuring that makes the Knight Cancer Institute into a self-governed entity within Oregon Health and Science University.
The move also brings back the OHSU cancer center’s longtime leader and star scientist Brian Druker, who will serve as the inaugural president of the new organization, called the Knight Cancer Group.
“That gives us the ability to align the responsibility of effectively spending this groundbreaking record setting gift with the authority to do that,” Druker said to The Cancer Letter. “We’ve become a little bit like a Fred Hutchinson or a Huntsman. We’re following in their footsteps and we’re really grateful to have this opportunity to continue to make an impact for patients with cancer.”
Montefiore Einstein Director Edward Chu dies of glioblastoma at 66
Nov. 21, 2025
Edward Chu was an expert in pharmacology whose research improved therapies for colorectal cancer, leading to the identification of new treatment targets and driving scientific advances in the field.
His understanding of cancer centers—how they are structured and how they operate—led many institutions to reach their highest potential. His ability to make complicated concepts seem simple was appreciated by medical students and directors of cancer centers. And, above all, he was a good guy, a really good guy, known for his wisdom, his wickedly funny, self-effacing sense of humor, and his infectious, full-throated laugh.
Chu, who improved every institution he worked in, directed, or advised while turning patients, trainees, and colleagues into friends, died of glioblastoma on Nov. 13. He was 66.
How MD Anderson and Texas Children’s made plans to build a $1 billion pediatric cancer hospital—one of the world’s largest
June 27, 2025
The windows down the hall from the operating room scrub sinks at MD Anderson Cancer Center look out at the tower of Texas Children’s Hospital.
Years ago, long before he became MD Anderson’s president, Peter WT Pisters often looked out those windows and thought of the possibilities for creating a massive pediatric oncology center by uniting the programs of his institution and those of Texas Children’s.
“I would be at the scrub sink, scrubbing with another surgeon. I would look out the window, and I would say to the person next to me at the sink, ‘Hey, why don’t we partner with them? They’re amazing,’” Pisters recalled recently.
The synergies were obvious. Both MD Anderson and Texas Children’s treat pediatric cancer, and their programs would fit together like pieces of a puzzle, Pisters thought. But obviousness notwithstanding, a joint project of this sort could never happen because it would require setting aside turf considerations, an alignment of political forces—and an extraordinary amount of time and resources.
“The community wanted something spectacular like this, but somehow it didn’t happen. We don’t know why. They all said it was impossible,” Pisters said.
And yet, last month, the forces aligned and the seemingly impossible project—called Kinder Children’s Cancer Center, a joint venture of the University of Texas MD Anderson Cancer Center and Texas Children’s Hospital—was ushered into existence. When it’s built, it will produce the largest children’s cancer hospital in the U.S. and one of the largest, if not the largest, in the world.
As fire encroached, City of Hope prepared to evacuate its Duarte campus
Jan. 10, 2025
On Jan. 7, a bit after 6 p.m., Ravi Salgia was at his Eaton Canyon home, at the edge of Angeles National Forest.
He was watching the news.
Like everyone else in Los Angeles, Salgia and his family were following updates on a wildfire driven by the Santa Ana winds as it raced through Pacific Palisades. Of course, the Palisades Fire was clear on the other side of Los Angeles, by the ocean.
Suddenly, his wife, Deborah, thought she saw a glow in the backyard. She looked out, then stepped outside into the back yard to get a better look. “And so, she saw the house above us on fire and flames coming down,” Salgia said. “And she said, ‘Honey, we’ve got to go.’
“We had five minutes. Otherwise, the flames would’ve engulfed us all. And so, we got in the car, only got the passports and marriage certificate, clothes on our back, and that was it—left everything behind. We were the first ones to evacuate from Eaton.”
When he spoke with this reporter two days after the hurried evacuation, Salgia, chair of the Department of Medical Oncology & Therapeutics Research and Arthur & Rosalie Kaplan Chair in Medical Oncology & Therapeutics Research at City of Hope, didn’t know whether his house was still standing.
Related:
- LA fires update: Salgia home is standing (The Cancer Letter, Jan. 17, 2025)
ACOG says it will no longer accept federal funding
Aug. 8, 2025
The American College of Obstetrics and Gynecology said it will no longer be accepting federal funding.
ACOG said this decision is due to federal policy changes that don’t align with the organization’s work. The organization said it may reconsider partnering at a federal level again in the future, should their “program goals align” with the government.
The ACOG Foundation—the group’s 501(c)(3) affiliate—has received $950,000 from HHS this year to oversee reviews and updates of preventive services guidelines for women, according to an HHS grant-tracking website. In 2023, the organization received over $1 million in federal funding.
FY25 paylines drop to 4th percentile—a historic low—as NCI braces for Trump’s FY26 budget cuts
July 25, 2025
NCI announced that the paylines for R01 grants for established and new investigators are expected to drop to the 4th percentile—a historic low for the institute.
In an update posted on the NCI website July 23, the institute said that it “will not establish a specific R01 payline for the remaining competing [Experienced Investigator/New Investigator] applications that have not yet been awarded for FY 2025,” but that they “expect to fund through the 4th percentile for those EI/NI applications.”
The fact that the percentile is not set opens the door to subjective review of all proposals before they are funded, observers said.
The Directors
In a new, monthly podcast series, The Cancer Letter interviews two directors of cancer centers about the problems that are keeping them up at night.


This series is sponsored by The American Society of Clinical Oncology.
On a new podcast, VCU’s Winn and City of Hope’s Carpten discuss the mission—and the future—of cancer centers
The Cancer Letter’s new podcast offers insight into cancer policy in a landscape of uncertainty
Feb. 14, 2025
Is the Community Outreach and Engagement mandate the next item on the chopping block as the Trump administration makes its mark on science policy? What about health disparities research?
“If we got rid of Outreach and Engagement, I think it would be almost like losing a major foundational aspect of a cancer center,” Robert A. Winn, the director at Virginia Commonwealth University Massey Comprehensive Cancer Center, said on The Cancer Letter’s new podcast. “And I think it would make us vulnerable, particularly in the public’s eye in saying, ‘Well, what do you exist for if it’s not for our benefit?’”
On the inaugural episode of The Directors, a series on The Cancer Letter Podcast, we asked Winn, a pulmonologist who holds the Lipman Chair in Oncology at VCU, and John Carpten, the chief scientific officer and director of City of Hope Comprehensive Cancer Center, and director of Beckman Research Institute, to imagine the future of the cancer centers without COE.
“We’ll lose our identity. It’s becoming our identity. And we’d lose it,” concurred Carpten, who holds the Irell & Manella Cancer Center Director’s Distinguished Chair at City of Hope and the Morgan & Helen Chu Director’s Chair of the Beckman Research Institute. “A tragedy. And I’ll just be honest, if that happens I would feel like I would have contributed to it and would be in part to blame, because we have to fight for this.
“It’s at the core of who we are supposed to be as a cancer center,” Carpten said.
“And so, I’m looking forward to standing shoulder to shoulder with Dr. Winn and the other cancer center directors to ensure that the engagement and involvement between the cancer centers and our communities has to be central to who we are and what we do.”
The Directors: Tom Lynch and Skip Burris on how NIH funding cuts imperil biopharma innovation—and cost patient lives
In a time of uncertainty, “react to the knowns, not the fear”
May 16, 2025
Thomas J. Lynch Jr. and Howard A. “Skip” Burris III lead two institutions that couldn’t be more different—an NCI-designated Comprehensive Cancer Center on one side of the country and a for-profit research enterprise on the other—but they stay up at nights worrying about the same thing:
“Changing the paradigm of how research is funded and how care is funded, I think makes us all a bit nervous,” said Lynch, president and director of Fred Hutch Cancer Center, an NCI-designated Comprehensive Cancer Center in Seattle.
“To stop that flow of ideas from universities and from hospitals to pharmaceutical companies, it is going to basically hand the future of biopharma to countries outside of the United States,” he said.
Burris, president of Sarah Cannon Research Institute, a for-profit community oncology research enterprise in Nashville, agrees.
“We’ve got a lot of work to do. But so many patients, so many new therapies, so many drugs. In that sense, the opportunities have never been greater,” Burris said.
“But on the other hand, we’ve got all the, as Tom uses the word, ‘uncertainty’—all this unrest, wondering how we’re going to be able to pay for this, how we’re going to be able to reimburse for various activities,” Burris said. “And really trying to have my team not get distracted and try to reassure them that financially we’re going to be okay, we’ve got to be diligent, we’ve got to think about how we handle those, but to really stay focused on the patients, the trials and the new drugs that are coming forward.
“And that’s been a bit of a challenge and more so of a challenge of late.”
The Directors: Steven Artandi and Eric Winer on how looming policy changes “reverberate” through oncology
“Even when funding gets restored and if the H-1B visa threat doesn’t materialize, it creates an environment where especially young people become uncertain.”
Oct. 10, 2025
With major leadership changes, grant disruptions and terminations, and a stoked distrust in science, Steven Artandi, the director of Stanford Cancer Center, worries that young investigators will feel disenchanted by the U.S. research atmosphere and take their work and study elsewhere.
“The uncertainty in the current system is giving some people pause, especially younger people, whether they’re Americans or whether they trained abroad, as to whether the United States is the right place to spend their careers,” said Artandi, who is also the Laurie Kraus Lacob Director of the Stanford Cancer Institute and the Jerome and Daisy Low Gilbert Professor of Medicine and Biochemistry at Stanford University. “So, I am up at night worrying about the future of American leadership in cancer science and in science more broadly.”
“And these changes reverberate,” said Eric Winer, director of Yale Cancer Center. “The fact that there’s this threat to scientists from around the world to be able to come to the U.S. is a real turnoff for a lot of people.”
There is an existential threat that the U.S. might not be the best place to do cancer research right now, said Winer, who is also president and physician-in-chief of Smilow Cancer Hospital, Yale New Haven Health System.
“This is the time where I think all of us in the field want to step hard on the research accelerator, we don’t want to back off,” Winer said.
However, Winer pointed out that he will not be the one making scientific discoveries in 10-20 years. It’s the future generations, the very ones who are feeling uncertain about entering into an unstable NIH, that worry him.
“And if we lose a generation, or even half a generation of people, it’s a huge problem for cancer medicine and cancer science,” Winer said.
The Directors: Mary Beckerle and Neli Ulrich on delivering cancer care across five states
Honoring the Jon Huntsman Sr. political perspective: “I’m not a member of any party except the Cancer Party”
Aug. 8, 2025
Mary Beckerle, a whitewater kayaker, has advice for all the folks in the cancer field: never catastrophize, never panic.
“Back in the day, I used to whitewater kayak, and you’ve got your paddle, and you’re in the water.
“And when you hit that rapid, the one thing you know you have to do is take that paddle and dig it into that wave and pull yourself through with gusto and with determination. And you can’t respond to this chop by just holding your paddle up in the air and going, ‘Uh-oh,’ or you lose every ounce of potential to shape the situation,” said Beckerle, who is also a cell biologist and CEO of Huntsman Cancer Institute.
Beckerle appeared on The Cancer Letter Podcast with Cornelia Ulrich, chief scientific officer and executive director at Huntsman, and Karen Knudsen, CEO of the Parker Institute for Cancer Immunotherapy and former CEO of the American Cancer Society.
“I think one of the things that we can think about in this time is that all of us need to think about digging in with that paddle, going directly into the middle of the wave that’s coming at us and shaping it as much as we can, and continuing to move forward rather than just being tossed and turned,” Beckerle said.
“And I think that’s a good image for what the scientific community is really trying to do right now.”
Related:
- Mary Beckerle to step down as CEO at Huntsman, succeeded by Brad Cairns (The Cancer Letter, July 11, 2025)
Top podcast episodes
The Cancer Letter’s weekly podcast series highlights the latest headlines, exclusive interviews, and more to dig deep into the issues that shape oncology, available on Spotify, Apple Podcasts, and YouTube.
Here are the top episodes:
Brian Druker on receiving a record-setting $2B gift to Knight Cancer Institute
Aug. 20, 2025
On Capitol Hill, NIH gets congressional support and RFK Jr. gets slammed,
Sept. 10, 2025
Gardiner Harris, acclaimed health care and pharma journalist, on his New York Times bestselling book
Aug. 27, 2025
What are Jay Bhattacharya’s plans for NIH?
March 12, 2025
Jonathan Mahler on his front-page story in the NYT Magazine on Trump’s deliberate dismantling of America’s War on Cancer
Sept. 17, 2025
Tidmarsh is out, Pazdur is in: FDA’s CDER under new leadership
Nov. 12, 2025
Is oncology ready to move away from animal testing?
July 23, 2025
Cancer history
In partnership with the Cancer History Project, The Cancer Letter’s historical initiative, some articles put contemporary headlines in their historical context, and others explore the impact of medical advances of their time. These selections appeared in the most-read stories this year.
Trump 2016: A look back at the 45th president’s impact on oncology
Nov. 8, 2024
As oncology contemplates the potential impact of a second Donald Trump term on cancer care and research, The Cancer Letter has compiled a list of guest editorials, news analyses, and data-driven reports that this magazine published during his first term.
Days after the 2016 election, there were uncertainties about President Barack Obama’s signature healthcare programs—the Affordable Care Act and the National Cancer Moonshot Initiative (The Cancer Letter, Nov. 10, 2016).
“We are in a historic time in cancer research,” Elizabeth Jaffee, co-chair of NCI’s Cancer Moonshot Blue Ribbon Panel, said to The Cancer Letter at the time. “We hope we will not lose the momentum.”
Ted Kennedy, RFK Jr.’s uncle, shaped the National Cancer Program. Will his nephew follow suit?
Jan 31, 2025
“The historic National Cancer Act of 1971 has often been called ‘Nixon’s War on Cancer,’ but it could as easily have been called ‘Kennedy’s War on Cancer,’ and with perhaps greater justification,” writes Richard Rettig, a historian of the National Cancer Act (The Cancer Letter, May 23, 2008).
Sen. Edward M. Kennedy, a democratic senator from Massachusetts, was one of three pivotal partners in the political dance that designed the National Cancer Program as we know it—Kennedy, President Richard Nixon, and renowned socialite and cancer advocate, Mary Lasker.
On Jan. 29, the Senate began confirmation proceedings for Robert F. Kennedy Jr., Ted Kennedy’s nephew and Trump’s nominee for secretary of the U.S. Department of Health and Human Services.
The Cancer History Project has collected an archive of Ted Kennedy’s impact on NIH, NCI, and cancer research.
Discovery of EGFR mutations dramatically changed lung cancer treatment
20th anniversary of landmark findings
By Suresh S. Ramalingam, MD, May 31, 2024
When I started fellowship training in the year 2000, the response from everyone when I mentioned my interest in lung cancer was nearly the same: “Are you sure?”
This experience was not unique to me; every thoracic oncologist at that time would likely relate to that. The basis was not hard to understand: lung cancer was a highly lethal disease, with practically one proven chemotherapy agent (platinum) that improved the 1-year survival rate by 10% for patients with stage 4 disease.
Even in uncommon situations where lung cancer was diagnosed at an early stage, survival was suboptimal despite complete resection. The stigma associated with tobacco smoking, lack of treatment options, and high mortality were driving the widespread nihilism for lung cancer.
It was not uncommon for patients to be directly referred to hospice following the diagnosis of lung cancer. In fact, the “Big Lung Trial” (published in 2004) compared platinum-based chemotherapy to best supportive care and demonstrated a 9-weeks improvement in median overall survival with the former. It hardly mattered if a patient had non-small cell lung cancer (NSCLC) (~85%) or small cell lung cancer (~15%).
It was during those days that I had the fortune of caring for patients on a clinical trial with an experimental targeted therapy, ZD1839. This small molecule was an inhibitor of the epidermal growth factor receptor (EGFR) which was overexpressed in a high proportion of patients with NSCLC.
Editor’s note: This story is part of a series
How the ancient Egyptians treated cancer
April 7, 2023
The first evidence of cancer—and cancer treatment—in humans dates back to the Pyramid Age, writes Jaya M. Satagopan, PhD, full member of the Cancer Prevention and Control Program at Rutgers Cancer Institute of New Jersey, and professor of biostatistics and epidemiology at Rutgers School of Public Health.
In her editorial about cancer in ancient Egypt, Satagopan explores a two-volume translation of papyrus that offers a glimpse into the first recorded evidence of cancer in humans: medical case studies of breast cancer dating back to 3000 BC.
This editorial accompanies her 2022 online museum exhibit published in the Cancer History Project about the history of cancer.
How Beth Carner went from six weeks left to live with stage 4 colon cancer to complete remission
June 10, 2022
At 25, Elizabeth Carner was diagnosed with stage 4 colon cancer.
“I mean, the first thing that went through my head was just looking at mom and dad, and it’s just like, OK, well, where did all the other stages go? Because we literally went from my colonoscopy as being OK to everything’s not OK,” Carner, now 33, said to Deborah Doroshow, an oncologist at the Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai.
At the time, Carner, who studied theater and stage management as an undergraduate, had a coveted job at an equity theater, Cincinnati Playhouse in the Park. She hadn’t thought much of her recent weight loss before the diagnosis—going from 175 to around 150—chalking it up to the hustle of theater life.
Then, one day, Carner fainted at work.
In 1971, Chris Lundy had minute odds of survival. He is now the longest living BMT recipient at the Hutch
Sept. 15, 2023
At 75, Chris Lundy is one of the longest living recipients of a bone marrow transplant.
He was among the patients included in the 1975 paper published in the New England Journal of Medicine titled “Bone-Marrow Transplantation.”
“It was a paper everyone interested in bone marrow transplantation read word for word,” Frederick Appelbaum, executive vice president, professor in the Clinical Research Division, and Metcalfe Family/Frederick Appelbaum Endowed Chair in Cancer Research at Fred Hutchinson Cancer Center, wrote in his book “Living Medicine.” “It was the article that introduced marrow transplantation to the general medical community.”
From The Cancer Letter archives
Some stories come back year after year, others come back when a recent headline resurfaces an older scandal, and others still seem to pop up into the zeitgeist with no rational explanation. Whatever the cause, we consider this The Cancer Letter’s hall of fame:
FDA grants Cytotron Breakthrough Device Designation for breast, liver and pancreatic cancers
Nov. 1, 2019
FDA granted Shreis Scalene Sciences Breakthrough Device Designation for the Cytotron, a CE-marked, whole-body therapeutic medical device.
Chernobyl: a 35 year follow up on long-term health effects
By Robert Peter Gale, MD, PhD, DSc(hc), FACP, FRCP, FRCPI(hon), FRSM, March 23, 2021
In the early morning of April 30, 35 years ago, I was awakened by a call from Anatoly Dobrynin, a long-time Soviet Ambassador to the United States.
He said General Secretary Mikhail Gorbachev wanted me to come to the Soviet Union to help treat victims of the Chernobyl nuclear power facility accident. I had cabled Gorbachev a few days earlier, offering my assistance.
Last year, I wrote a series of reviews of the HBO Chernobyl miniseries in The Cancer Letter, discussing acute health effects of exposure to acute high dose ionizing radiations, and correcting some inaccuracies in the TV series.
Now, with 35 year follow-up, I update what we know about the long-term health effects, especially cancer risk.
Related:
- Chernobyl, the HBO miniseries: Fact and fiction (The Cancer Letter, four-part series)
The unKOOL, unfiltered history of menthol cigarettes
By Alan Blum, MD, May 7, 2021
Quick, what color is menthol?
No, it’s not green. That’s the color of the KOOL, Newport, or Salem cigarette pack. Get it? Green is cool. Red is hot.
Menthol, a component of peppermint oil, is a colorless topical pain reliever like Novocain that the dentist uses to numb a tooth.
The idea of adding menthol to reduce smoking’s harshness on the throat came to Lloyd “Spud” Hughes in the 1920s, after he’d stored his cigarettes in an old tin of menthol crystals that his mother insisted that he inhale for his asthma.
He patented the process in 1924, and three years later, the Axton-Fisher Tobacco Company acquired the patent and began manufacturing “Spud Menthol Cooled Cigarettes.”
Today, as the Biden administration targets mentholated cigarettes, it behooves us to review the history of the tobacco industry’s marketing campaigns that target Black Americans.
Gynecology’s deadly surprise: Cancers are frequently missed prior to routine procedures
May 18, 2018
As they reach for surgical tools, gynecologists vastly underestimate the probability that their patients have undiagnosed uterine cancers, a study by Yale University researchers found.
Their paper, published in Obstetrics & Gynecology last month, is immediately relevant in the clinic, because a suspicion that cancer may be present dictates the choice of surgical techniques employed in gynecological procedures that are performed in about 650,000 women every year in the United States.
The newly calculated prevalence rates, based on analysis of data from 26,444 cases in the 2014-2015 American College of Surgeons National Surgical Quality Improvement Program, are staggering:
One in 20 women over age 55 were subjected to surgery for benign indications, but were later found to have malignancies in the main body of the uterus. Nearly one in 10 women over age 55 who underwent total abdominal hysterectomies had hidden corpus uteri cancer.
Overall, prevalence of cancers undetected at the initiation of hysterectomies was almost as high as one in 70. For women who underwent total laparoscopic or laparoscopic-assisted vaginal hysterectomies, the estimated prevalence rose to nearly one in 50.
Related:
- When Surgical Innovation Kills (The Cancer Letter, series)
- Amy Reed, physician and patient who “moved mountains” to end widespread use of power morcellation, dies at 44 (The Cancer Letter, May 26, 2017)
Trump et al. are wrong: Biden Cancer Initiative is not to be confused with the Beau Biden Cancer Moonshot
Nov. 16, 2020
On Nov. 15, shortly after midnight, President Donald J. Trump tweeted a link to a New York Post headline:
“Tax filings reveal Biden cancer charity spent millions on salaries, zero on research”
Waking up later that morning, Fox News host Laura Ingraham and former Trump campaign manager Corey Lewandowski, gleefully lent their voices to the now-familiar cacophony of disinformation. A day later, Fox News host Sean Hannity joined their chorus.
For those just tuning in, the president was retweeting a story about the Biden Cancer Initiative, a small organization that is not to be confused with the Beau Biden Cancer Moonshot, a bipartisan effort to increase funding for cancer research.
Should you eat a kielbasa tonight?
Six experts weigh evidence on papers debunking nutritional guidelines on red and processed meat
Oct. 4, 2019
We asked six experts in disease prevention, nutrition, and guidelinemaking to discuss the just-published recommendations that disagree with the dietary guidelines promulgated by mainstream health organizations.
The paper, published in Annals of Internal Medicine said there is little evidence of increased risk of cancer, heart disease, and other harm from eating red meat and processed meat.
Vinay Prasad, oncologist and Twitter star, locked in debate over precision medicine
June 22, 2018
In recent years, Vinay Prasad, a young hematologist–oncologist at Oregon Health and Science University, has emerged as a premier critic of new directions in cancer medicine.
In his view, cancer drugs are aimed at miniscule populations, approved way too easily, and priced too high.
With nearly 21,300 Twitter followers, over 30,000 tweets, a book, and multiple op-eds, Prasad can turn an academic paper into a bestseller—and an obscure point into a rallying cry.
Vinay Prasad is the guy to call.
“He has positioned himself as the iconoclast/John Ioannidis model for oncology. That was how he floated to the top,” said Jeremy Warner, associate professor of medicine and biomedical informatics at Vanderbilt University and ASCO 2018 Annual Meeting Education Committee track leader of the Health Services Research, Clinical Informatics, and Quality of Care track.
Related:
- Cyber-iconoclast Vinay Prasad named head of FDA’s CBER (The Cancer Letter, May 9, 2025)
- Vinay Prasad named chief medical and scientific officer at FDA (The Cancer Letter, June 20, 2025)
- Right-wing provocateur Laura Loomer comes for FDA’s Vinay Prasad (The Cancer Letter, July 25, 2025)
- Vinay Prasad falls from grace at FDA upon flunking Trump political purity test (The Cancer Letter, Aug. 1, 2025)
- The departure (and return) of Vinay Prasad (The Cancer Letter, Sept. 5, 2025)
- Vinay Prasad regains role as FDA chief medical and scientific officer (The Cancer Letter, Sept. 12, 2025)
Prominent GI oncologist Axel Grothey was forced out of Mayo Clinic for unethical sexual relationships with women he mentored
Three reprimands later, he retains leadership—and mentorship—positions
May 28, 2021
The aftermath of sexual misconduct at premier medical institutions rarely leaves visible traces: HR is brought in, confidentiality invoked, deals made. The case of Axel Grothey’s exit from Mayo Clinic is a notable exception.
Last year, the prominent gastrointestinal oncologist was reprimanded by medical licensure boards in three states for engaging in unethical sexual relationships with an oncology fellow and a faculty colleague at Mayo Clinic Rochester, his longtime place of employment.
Three reprimands notwithstanding, Grothey has kept his appointment as co-chair of the NCI National Clinical Trials Network’s Gastrointestinal Steering Committee, an influential group that reviews ideas for clinical trials and helps determine the priorities in federally funded clinical research in GI oncology.
Editor’s note: This story is part of a series.