Albert de la Chapelle, a Distinguished University Professor at The Ohio State University and a giant in the field of genetics, died Dec.10, 2020, after a short bout of pneumonia while visiting his home in Finland.
He was married to the renowned leukemia researcher, Clara D. Bloomfield, who died in March 2020 (The Cancer Letter, March 6, 2020). He was in Finland to carry out one of her final wishes—to place half of her ashes where she had grown up in Illinois, and half in Finland at the home where they had spent their summers.
We know he was at peace having fulfilled this important obligation before his own death.
Both members of the National Academy of Sciences, this formidable couple had been married for 38 years and worked on different continents for the first 15 until they moved to Ohio in 1997. When de la Chapelle turned 65, the mandatory retirement age in Finland, he and Bloomfield took it as an opportunity to relocate together.
At the time, she was recruited to The Ohio State University to serve as the director of the OSU Comprehensive Cancer Center. He was the “trailing spouse” brought in by leadership to build a Human Cancer Genetics program, who sensed that cancer genetics was the future of oncology. De la Chapelle often said that they “found their little spot of heaven in Delaware, Ohio,” on the 40 acre property they purchased and lived in for the past 23 years.
“In August of 1997, I was introduced to Dr. Albert de la Chapelle when he hired me over the telephone, sight unseen, to join the Human Cancer Genetics Program at The Ohio State University which he had just been tasked with building from scratch,” said Heather Hampel, associate director of the Division of Human Genetics, associate director of biospecimen research, professor of internal medicine, and licensed genetic counselor of OSUCCC – James.
“I was a young cancer genetic counselor who had grown up in Ohio and wanted to come home to my alma mater. For the past 23 years, he was my mentor. He taught me how to do translational research in cancer genetics and how to lead quietly by example,” she said.
De la Chapelle was a great lover of nature and their property teamed with wildlife, daffodils, and Christmas trees that he grew himself. For many years, he would invite members of the Human Cancer Genetics program to cut down their own Christmas trees from his yard.
At one point, de la Chapelle commissioned an archeological study of the property, at a location that was used by Native Americans. The results and some of the tools discovered were published in a book about the property.
De la Chapelle cared deeply for animals; lamenting the fate of turkeys on Thanksgiving, the Canadian geese hit on the side of the road, and deer fawn born out of season on his property.
He went to Tasmania to see the Tasmanian devils and offered to stay to help study the facial tumor disease that had decimated the population. Luckily, a government-funded initiative was already in place to save the Tasmanian devil, so his offer was declined—or else we might have missed a few years of his human genetics research. Nevertheless, he was the proud patron of a Tasmanian devil at the Columbus Zoo.
Lynch syndrome
De la Chapelle was born Feb. 11, 1933 in Tenala, Finland and was named for his grandfather, who was a pediatrician. As his namesake, it was expected that he would receive a medical degree, which he did in 1957 from the University of Helsinki.
He was later board certified in internal medicine. During his medical training, de la Chapelle became interested in genetic conditions after reading a paper linking Turner Syndrome with monosomy X written by one of his professors. This ultimately led de la Chapelle to pursue a PhD and conduct his own research in the cytogenetics of sex determination.
In 1962, he earned his PhD in Human Genetics with a thesis project focusing on Turner Syndrome. He continued his work on the identification and characterization of sex chromosome anomalies including his discovery of a male with two X chromosomes which he described in 1964.1
After finding evidence of recombination between the two chromosomes, he ultimately identified the pseudoautosomal regions on the X and Y chromosomes2. His work with sex chromosome anomalies even affected policies by the International Olympic Committee. Beginning in the late 1960s, the sex chromosome and PCR-based tests misidentified women with specific mutations as male. Women so mislabeled were prevented from competing and suffered emotional consequences. De Chapelle, together with other scientists, called out this practice—resulting in discontinuation of this testing in 19983.
For the past 23 years, he was my mentor. He taught me how to do translational research in cancer genetics and how to lead quietly by example.
Heather Hampel
In the early 1980s, de la Chapelle wanted to move from cytogenetics into molecular genetics and spent a year with Dr. Jean-Claude Kaplan at the University of Paris, and two years in the laboratory of Paul Marks at Columbia University.
This led to his eventual transition into the world of cancer genetics while still in Finland. De la Chapelle’s team was the first to describe microsatellite instability and its relationship with Lynch syndrome in 19934. They subsequently linked the MSH2 gene responsible for Lynch syndrome to chromosome two5.
Just before leaving Finland, his team had shown that MSI could be used to screen colorectal cancer patients for Lynch syndrome and follow-up genetic testing estimated that 2.8% of all colorectal cancers were due to Lynch syndrome. There were many founder mutations in Finland, including two in the MLH1 gene, which made him wonder if the prevalence of Lynch syndrome was the same in other populations.
After arriving at OSU, de la Chapelle wanted to repeat the study with a larger cohort of colorectal cancer patients and include endometrial cancer patients. When first applying for NCI funding, the grant was not funded because the reviewers felt Americans would not be willing to enroll in a study that included genetic testing—out of fear of genetic discrimination.
De la Chapelle was not dissuaded—he and his team moved forward and started the study anyway, and reapplied six months later when several hundred patients had been enrolled, evidence that such a study was feasible in the U.S.
Five years later, with 1,566 colorectal cancer patients and 562 endometrial cancer patients enrolled, the team found that around 2.8% of both of these cancers were due to Lynch syndrome, just as he had found in Finland6.
More importantly, the researchers proved that universal tumor screening for Lynch syndrome was feasible, and it is now the standard of care around the world, with professional organizations recommending it for colorectal and endometrial cancer patients.
Implementation has been slower than desired, which led to the recent Ohio Colorectal Cancer Prevention Initiative study (2013-2017), enrolling >3,300 colorectal cancer patients from 51 hospitals throughout the state of Ohio, in the largest universal tumor screening study to date.
Translational research
De la Chapelle truly loved translational research. His lab meetings were always attended by clinicians and the laboratory team. It was very important for those in the lab to understand the phenotypes of the patients so they could understand the underlying genotypes.
It was equally important for the clinicians to understand what was being found in the laboratory in case it could be explained by clinical information. His goal was not just to find genes, but to help people. This is why it was very personally fulfilling for him to be part of the important 2015 research study from Luis Diaz’ group at Johns Hopkins, which found that patients with microsatellite unstable tumors responded well to immune checkpoint inhibition therapy7.
“Dr. de la Chapelle cared deeply about finding answers for families with cancer. His enormous contributions to the field were rooted in that purpose,” said Pamela Brock, associate professor within the Division of Human Genetics in the Department of Internal Medicine at The Ohio State University College of Medicine.
De la Chapelle also made milestone contributions to the field of acute myeloid leukemia genetics. Being especially fond of abnormalities including chromosomes 7, 8 and 21, and also his all-time favorite Y chromosome, he reported monosomy 7 in myelodysplastic syndromes, as well as its association with diabetes insipidus, and specific partial aberrations.
Almost 30 years later, de la Chapelle still helped to uncover monosomy 7 in AML, together with Bloomfield, by defining associated gene expression signatures and mutated genes. In chromosome 8 associated studies, he discovered the gene BAALC whose high expression is associated with poor AML outcomes, as well as several AML-associated microRNAs, including miR-3151 and miR-3662.
Being again ahead of his time, de la Chapelle utilized clonal chromosomal abnormalities to show multi-lineage involvement in AML.
Additional studies
De la Chapelle also participated in and led collaborative studies on the genetic susceptibility to AML. Together with his wife Clara, and in close collaboration with his friend Julius Gudmondson at DeCode in Iceland, he spearheaded the first large-scale genome-wide association study in AML that led to the identification of a polymorphism near the BRD4 Interacting Chromatin Remodeling Complex Associated Protein (BICRA) gene as first AML risk variant.
He also remained actively involved in the studies of recurrent chromosomal abnormalities, and the identification of leukemia-associated genes and gene mutations. In addition to his studies in AML, he also passionately studied chronic lymphocytic leukemia with special focus on the discovery of predisposing genes and variants in individual families and large patient cohorts.
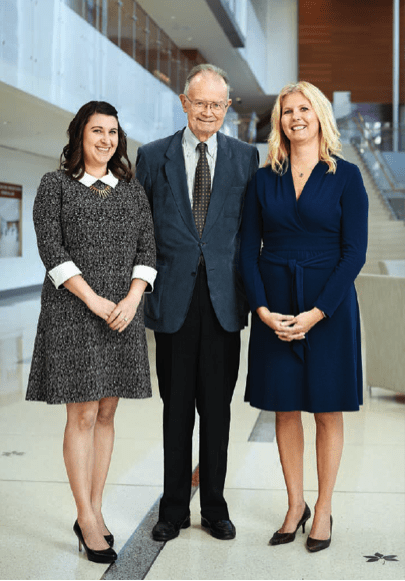
L-R: Rachel Pearlman, MS, LGC, Albert de la Chapelle, MD, PhD, and Heather Hampel, MS, LGC
In recent years, de la Chapelle became intrigued by the genetics of non-medullary thyroid cancer, which is one of the most heritable cancers, with no strong susceptibility genes identified. NMTC also has a significant sex difference with females affected three times more often than males.
“Albert was truly a giant in the field of genetics,” said Matthew Ringel, director of the Division of Endocrinology, Metabolism and Diabetes at The Ohio State University. “From the time of my recruitment to OSU when he asked me if I had ‘noticed that papillary thyroid cancer occurred in families’ in my own clinical practice, to our long-term collaboration in thyroid cancer predisposition and biology—his interests were not only in science and genetics, but also in mentoring and sharing a personal connection with his students and collaborators.”
“He will be deeply missed for his continuing scientific contributions, mentorship, and friendship,” said Ringel, who holds the Ralph W. Kurtz Chair in Hormonology and is co-leader of the Cancer Biology Program at the OSUCCC – James.
This reminded him of his early work on sex chromosome aneuploidies—and he always liked a good challenge. For many years, he oversaw the recruitment of families with individuals with NMTC from across the country and the world.
His lab identified several candidate genes for familial NMTC, including a highly penetrant private mutation responsible for papillary and anaplastic thyroid cancer in a large kindred from Kentucky. His team also conducted GWAS experiments with colleagues in Iceland and found several single nucleotide polymorphisms with strong associations to thyroid cancer8.
These findings led to the development of a polygenic risk score for thyroid cancer risk, as well as other important advancements in the understanding of this complex disease. His lab was still busy working on the genetics of thyroid cancer at the time of his death.
Legacy
De la Chapelle received prestigious awards and honors for his important scientific contributions6. He became a member of the National Academy of Science for his work in linkage and positional cloning to identify genes important in Mendelian-inherited disease in 1997. In 2002, he received the William Allan Award from the American Society of Human Genetics for substantial lifetime contributions to the field of human and medical genetics.
“Dr. de la Chapelle was always very encouraging and interested in the science. I remember when I was interviewing for a faculty position at OSU for the human cancer genetics program. When we were leaving the conference room following my job seminar, Dr. de la Chapelle asked me, ‘Tell me, Dr. Toland, are there any examples of gene-gene interactions important in cancer?’ I said, ‘Not, yet. But I hope to find some.’ He gave me a smile and said, ‘I look forward to hearing about them,’” said Amanda Toland, associate professor of cancer biology and genetics at The Ohio State University, and a member of the Molecular Carcinogenesis and Chemoprevention Program at the OSUCCC – James.
Dr. de la Chapelle cared deeply about finding answers for families with cancer. His enormous contributions to the field were rooted in that purpose.
Pamela Brock
De la Chapelle was honored by membership to its senior Academy of Sciences on Letters in Finland and was named a fellow in the Academy of Finland. He was also a Member of the Royal Swedish Academy of Sciences.
In 2017, the Collaborative Group of the Americas on Inherited Gastrointestinal Cancer awarded him a lifetime achievement award for his seminal contributions to our understanding of Lynch syndrome.
De la Chapelle had no children of his own, yet his pedigree is large, comprised of the fellows, students, genetic counselors, and other trainees that he mentored over the years.
“When I sent Dr. de la Chapelle a manuscript, he worked right away and returned the revised version quickly,” said Huiling He, research scientist in the de la Chapelle lab at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute. “He liked using a pencil to jot down his words on the manuscript or add a paragraph on a sheet of paper. Then he went over with me page-by-page and explained why he made each change. His eyes were so sharp to spot typos, incorrect grammar, or inaccurate expressions.”
Over the years, de la Chapelle mentored individuals who have become notable cancer genetics researchers in their own right: Juha Kere, Lauri Aaltonen, Ralf Krahe, Laura Valle, Paivi Peltomaki, Hidewaki Nakagawa, Christoph Plass, Natalia Pellegata, and Krystian Jazdzewski. They have in turn, mentored others—and thus his legacy continues.
Describing his mentorship, “It would be first of all his unconditional friendship and support for the fellow as a person, and for their scientific ideas and goals, from big to small,” said Ann-Kathrin Eisfeld, assistant professor in the Division of Hematology at The Ohio State University and a member of the Leukemia Research Program at the OSUCCC – James.
“It would be his unstoppable curiosity, which included lively discussions about the smallest details of geographic points and local traditions from the fellows’ hometowns, and, of course, his curiosity for everything in science and biology, even if it was far off his own research interest,” Eisfeld said. “Finally, it would be his unparalleled ability to see the big picture, find the one small detail that matters, and think big in every project. Already now, I deeply miss his kindness, and the feeling that anything is possible when walking out of his office, or house, after our meetings.”
We are all better for having known de la Chapelle—better researchers, better collaborators, better listeners, and better people.
References:
de la Chapelle A., Hortling H., Niemi M., Wennström J. XX sex chromosomes in a human male: first case. Acta. Med. Scand. Suppl. 1964; 412: 25–38.
de la Chapelle A. The use and misuse of sex chromatin screening for “gender identification of female athletes. JAMA. 1986; 256: 1920-1923.
Aaltonen L.A., Peltomäki P., Leach F.S., Sistonen P., Pylkkänen L., Mecklin J.P., Järvinen H., Powell S.M., Jen J, Hamilton S.R., et al. Clues to the pathogenesis of familial colorectal cancer. Science. 1993; 260:812-6..
Peltomäki P., Aaltonen L.A., Sistonen P., Pylkkänen L., Mecklin J.P., Järvinen H., Green J.S., Jass J.R., Weber J.L., Leach F.S. Genetic mapping of a locus predisposing to human colorectal cancer. Science. 1993; 260: 810–812.
Hampel H., Frankel W.L., Martin E., Arnold M., Khanduja K., Kuebler P., Nakagawa H., Sotamaa K., Prior T.W., Westman J. et al. Screening for the Lynch syndrome (hereditary nonpolyposis colorectal cancer). N. Engl. J. Med. 2005; 352: 1851–1860.
Le D.T., Uram J.N., Wang H., Bartlett B.R., Kemberling H., Eyring A.D., Skora A.D., Luber B.S., Azad N.S., Laheru D., et al. PD-1 Blockade in tumors with mismatch-repair deficiency. N. Engl. J. Med. 2015; 372:2509-20.Printz C. First person profile: Albert de la Chapelle, MD, PhD. Cancer. 2019; 125: 3285-3286.
Gudmundsson J, Thorleifsson G, Sigurdsson JK, Stefansdottir L, Jonasson JG, Gudjonsson SA, Gudbjartsson DF, Masson G, Johannsdottir H, Halldorsson GH, et al. A genome-wide associate study yields five novel thyroid cancer risk loci. Nat Commun. 2017;8:14517.