- Podcast: Chris Lundy had one week to live; 52 years later, he is the longest living BMT recipient at the Hutch | Sept. 15, 2023
At 75, Chris Lundy is one of the longest living recipients of a bone marrow transplant.
He was among the patients included in the 1975 paper published in the New England Journal of Medicinetitled “Bone-Marrow Transplantation.”
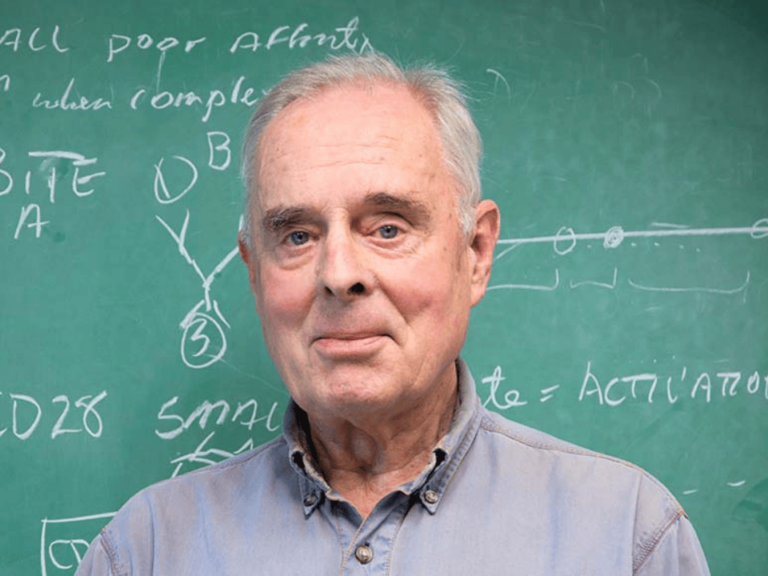
“It was a paper everyone interested in bone marrow transplantation read word for word,” Frederick Appelbaum, executive vice president, professor in the Clinical Research Division, and Metcalfe Family/Frederick Appelbaum Endowed Chair in Cancer Research at Fred Hutchinson Cancer Center, wrote in his book “Living Medicine.” “It was the article that introduced marrow transplantation to the general medical community.”
An interview and podcast with Appelbaum about his book “Living Medicine,” is available on the Cancer History Project.
Lundy’s path to diagnosis and treatment was not simple. At age 18, during basic training in Fort Polk, LA, Lundy slipped and broke his wrist.
At the hospital, the doctors set his wrist and ran some blood tests. What Lundy thought would be a simple visit turned into an eight-month stay.
“What they found was that I had an extremely low hematocrit,” Lundy said to Deborah Doroshow, assistant professor of medicine, hematology, and medical oncology at the Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai. “I was jaundiced, I had double walking pneumonia, and I was a pretty sick puppy. And if I hadn’t broken my wrist and gone to the hospital, I probably wouldn’t have been around too much longer—because I think my hematocrit was about four and a half or five, and normal was supposed to be up around 15.”
Doroshow, who is also a historian of medicine, is a member of the editorial board of the Cancer History Project.
Doctors at the hospital in Fort Polk thought Lundy had a reactionary hemolytic anemia, but it took them a while to settle on an initial diagnosis. They conducted several bone marrow biopsies, took blood for testing, and began treating Lundy with prednisone—the hope being that this might jumpstart his red blood cell count. Nothing seemed to work.
“I felt like a big pin cushion,” Lundy said.
After eight months, they transferred him to a hospital in Fort Sam Houston, TX. There, doctors determined that Lundy had paroxysmal nocturnal hemoglobinuria.
“In the medical books, there were literally about four sentences after the name, and that’s about all they had,” he said. “I was, like, the 800th recorded case of someone having this.”
The suspected cause?
In Fort Polk, recruits going through basic training were moved out to the football field and put in tents. The tents were sprayed with insecticide.
“I had been sprayed with insecticide, and the insecticide had stopped me from making blood,” Lundy said.
Lundy spent 38 months in the hospital. During that time, he contracted pneumonia 34 or 35 times.
“You can have a sniffle, and I would get pneumonia,” he said.
Due to his weakened immune system, Lundy wasn’t allowed many visitors, and spent a lot of time on his own.
“Now if someone is in a room, you have some different things that you can entertain yourself with—like radio, tv, etc. I didn’t have any of those things,” he said. “I got a paint-by-number set. I got a couple of coloring books. I got a couple of paperback books from the cart that went around, but anything that came in the room had to stay in the room.
“And anything that came in the room had to be treated, or radiated before it came into the room so that it didn’t bring bugs with me, or with it.”
In Fort Sam Houston, Lundy’s doctors exhausted his treatment options, recommending that he go to Fred Hutch Cancer Center in Seattle.
“It turned out to be a good thing because that’s where I met Dr. [E. Donnall Thomas, who later was in charge of doing the transplant,” Lundy said. Thomas would share the Nobel Prize in Physiology or Medicine in 1990 for discoveries concerning organ and cell transplantation in the treatment of human disease.
In Seattle, Lundy enrolled in junior college, began living in his own apartment, and continued to have his blood evaluated.
“We did a quick routine that kind of jolted the system, and my system responded, and it started making blood cells again, and things were looking very rosy,” he said.
Lundy’s doctors gave him the OK to embark on a project—he began to build a fiberglass hatch to make an aquarium.
“Two days later, I’m doing this application, within 24 hours, my blood counts plummeted,” he said. “It went like a vertical drop, and I felt terrible…That was the beginning of the worst times, if you will, because I never really recovered from that incident.”
As Lundy’s blood counts dropped, his doctors had been looking at the possibility of a bone marrow transplant. The procedure was new, dangerous, and uncertain.
The following year was marked by frequent hospital stays and illness—at one point running a fever of 106 for about a week. At one point not long before the transplant, Lundy was confined to his hospital bed 24/7.
One day in 1971—five years after Lundy’s initial diagnosis—a doctor came into his hospital room, offering him good news and bad news.
The good news?
“‘We’ve decided that we’re going to try and do the bone marrow if you want to,’” the doctor told Lundy. “‘The estimate is that you probably only have a 10% chance of pulling through it.’”
The bad news? Lundy only had a week to live if he decided not to go through with the bone marrow transplant.
“At that point, the world felt really heavy,” Lundy said.
The doctors HLA-typed Lundy’s family and determined that his brother, Jerry Lundy, was a match. Jerry agreed to be a donor and Chris decided to go through with the transplant.
“I was fine. No graft versus host disease, no hiccups or bumps in the road. I just sailed right through it in terms of all the things they thought could happen, might happen, and none of that did,” he said.
Jerry, however, experienced complications—while doctors and nurses took blood from Jerry, he went into cardiac arrest. The medication they had given him for the procedure, protamine, was determined to be the cause.
“It happened three days in a row, the same thing,” Jerry Lundy said. “First day they shot it all in and I went into cardiac arrest. And then the next day they spread it out over a period of time, and I still went into cardiac arrest. And the third day they did the same thing, and did it again.”
After the third time, doctors released Jerry Lundy without giving him the coagulant.
“[They] just let me go with my blood thin,” he said. “I couldn’t shave, couldn’t go nowhere. I couldn’t do nothing that I would take a chance on cutting myself, because I would’ve bled out.”
Complications aside—the transplant was a success. In 1972, Lundy returned to school. He went on to have a career as a middle and high school teacher.
“For the most part, I’ve always felt like it was a part of my life,” Lundy said. “Because I was number 29 to have the transplant, it turns out, as the years go by, I am longer-living.”
Chris and Jerry Lundy spoke with Deborah Doroshow.
This column features the latest posts to the Cancer History Project by our growing list of contributors.
The Cancer History Project is a free, web-based, collaborative resource intended to mark the 50th anniversary of the National Cancer Act and designed to continue in perpetuity. The objective is to assemble a robust collection of historical documents and make them freely available.
Access to the Cancer History Project is open to the public at CancerHistoryProject.com. You can also follow us on Twitter at @CancerHistProj, or follow our podcast.
Is your institution a contributor to the Cancer History Project? Eligible institutions include cancer centers, advocacy groups, professional societies, pharmaceutical companies, and key organizations in oncology.
To apply to become a contributor, please contact admin@cancerhistoryproject.com.