Early endpoints have the potential to get effective drugs to patients faster, but granting approval to drugs—even accelerated approval—comes with the risk that ineffective or even harmful drugs will be given to patients.
This episode is available on Spotify and Apple Podcasts.
“If we don’t have these intermediate endpoints to get new drugs to patients, we’d have to wait… I think somebody mentioned in one of the conversations I had while I was reporting on this, that the readout would be upwards of 17 years to get information about these new drugs that are being developed if we rely on PFS, overall survival, the sort of traditional clinical endpoints,” Jacqurelyn Cobb, associate editor of The Cancer Letter, said, “So, that’s sort of the general push, to make it so effective drugs, can get it to patients faster. Now, with that, of course, comes a lot of risks. And that’s the balance, the conversation. That’s why this is something that’s so fun to cover.”
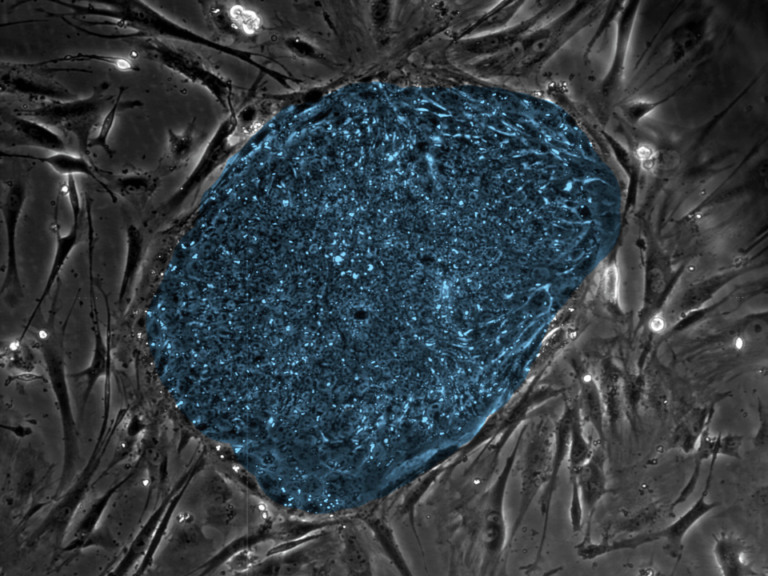
In this episode of In the Headlines, Jacquelyn and Paul Goldberg, editor and publisher of The Cancer Letter, talk about Friends of Cancer Research’s ctMoniTR project, a large-scale effort that aims to improve the efficiency of the development of intermediate endpoints.
The ctMoniTR project aims to learn and improve upon previous development of early endpoints, such as minimal residual disease, which is now an accepted early endpoint for the accelerated approval multiple myeloma.
Jacquelyn and Paul also talk through Paul’s story about the new director of the National Institute of Environmental Health Sciences, and Jacquelyn’s story about the recent results from GRAIL’s PATHFINDER 2 study, which is intended to support an FDA premarket approval application.
Stories mentioned in this podcast include:
- Friends study points to ctDNA’s potential to serve as an intermediate endpoint in NSCLC ctMoniTR project aims to improve efficiency in development of intermediate endpoints
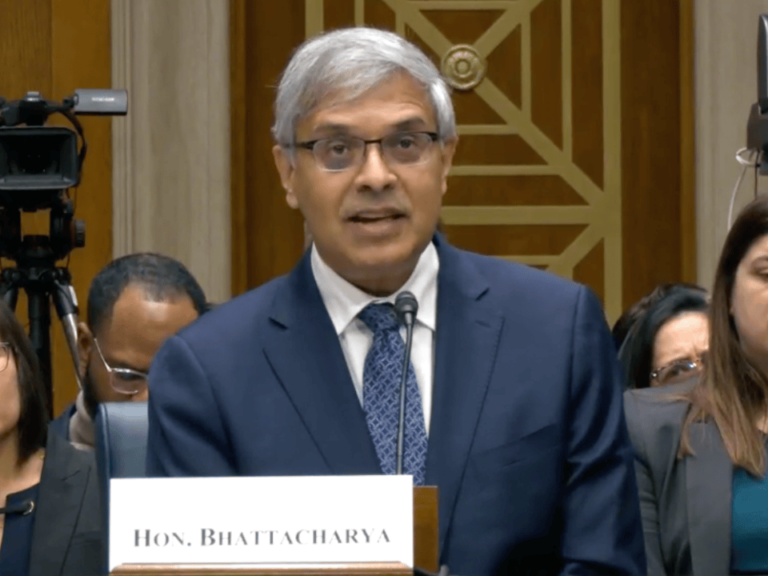
- Duke brain cancer researcher Kyle Walsh named director of NIEHS
- GRAIL to use new study results to seek FDA approval of Galleri MCD test
- Omar Abdel-Wahab, John Byrd, Lieping Chen, Robert Ferris, Wendy Garrett, Victor Velculescu are among new members of National Academy of Medicine
- Experts warn that loss of carcinogen surveillance threatens to increase cancer incidence
This episode was transcribed using AI transcription services. It has been reviewed by our editorial staff, but the transcript may be imperfect.
The following is a transcript of this week’s In the Headlines, a weekly series on The Cancer Letter podcast:
Jacquelyn Cobb: This week on The Cancer letter Podcast…
If we don’t have these intermediate endpoints to get new drugs to patients, we’d have to wait… I think somebody mentioned in one of the conversations I had while I was reporting on this, that the readout would be upwards of 17 years to get information about these new drugs that are being developed if we rely on PFS, overall survival, the sort of traditional clinical endpoints. So, that’s sort of the general push, to make it so effective drugs, can get it to patients faster. Now, with that, of course, comes a lot of risks. And that’s the balance, the conversation. That’s why this is something that’s so fun to cover.
Paul Goldberg: You’re listening to The Cancer Letter Podcast. The Cancer Letter is a weekly independent magazine covering oncology since 1973. I’m your host, Paul Goldberg, editor and publisher of The Cancer letter.
Jacquelyn Cobb: And I’m your host, Jacquelyn Cobb, associate editor of The Cancer letter. We’ll be bringing you the latest stories, groundbreaking research and critical conversations shaping oncology.
Paul Goldberg: So let’s get going.
Jacquelyn Cobb: Hey, Paul. How’s it going?
Paul Goldberg: Doing great, Jacquelyn. I can’t believe another week has gone by.
Jacquelyn Cobb: I know, I know. And last week was pretty crazy. My brain is still tired. So we have a lot to talk about today.
Paul Goldberg: Yeah, yeah. You’re writing so much it’s almost scary.
Jacquelyn Cobb: Scary. Is that a Halloween joke?
Paul Goldberg: It’s a Halloween joke. No, no. You’re doing a wonderful job. You’re making things that are difficult to understand, easier to understand even for feeble minds like mine.
Jacquelyn Cobb: That’s my job. No, I’m just kidding.
Paul Goldberg: So, we should have… Here’s where we screwed up. We should have been in costume.
Jacquelyn Cobb: I know. I know. I don’t even have a costume yet and it’s coming. The weekend’s coming.
Paul Goldberg: See, I would’ve been a clown. Maybe a sad clown.
Jacquelyn Cobb: A sad clown is probably the most depressing costume I could possibly think of. What do you mean, a sad clown?
Paul Goldberg: Well, I like dark comedy. The sad clown is a pretty funny thing.
Jacquelyn Cobb: Yeah, if you’re going to go dark humor. All right. Well, let me take us through the headlines before we go further down the deep end. I wrote the cover story last week about the Friends of Cancer Research’s ctMoniTR project. It is a large-scale effort that aims to improve the efficiency of the development of intermediate endpoints. We’re going to go through that in more detail later in the podcast. And then Paul wrote a story about the new director of the National Institute of Environmental Health Sciences, and I wrote a story about the recent results from GRAIL PATHFINDER 2 study, which I think we’re also going to be talking about, so I’m not going to give too much detail there.
And we had a story about the new members of the National Academy of Medicine, just sort of a list of oncology-related people. And finally, we had a guest editorial by members of the Environmental Mutagenesis and Genomics Society about the importance of carcinogen surveillance. So that was a really interesting story too. But I think we’re going to be getting sort of deep into three of these stories, so I wanted to keep this brief this week since we’ll be talking about them.
Paul Goldberg: Well, we should talk about intermediate endpoints first. It’s really interesting. So we’re talking about solid tumors, specifically non-small cell lung cancer, and it’s been used for multiple myeloma and AML.
Jacquelyn Cobb: ALL.
Paul Goldberg: ALL. Excuse me. And it’s being used for hematologic malignancies, specifically multiple myeloma and ALL. So ta-da, what’s different now?
Jacquelyn Cobb: Yeah. I mean, just to give some context, I mean the really broad narrative here is that treatments are getting better and there are sort of other nuances, but basically, people are either living longer or responding to a lot of different drugs now. This is happening in the myeloma space.
There was an ODAC I think earlier this year that focused on MRD minimal residual disease, in myeloma or multiple myeloma. And yeah, it’s basically if we don’t have these intermediate endpoints to get new drugs to patients, we’d have to wait… I think somebody mentioned in one of the conversations I had while I was reporting on this, that the readout would be upwards of 17 years to get information about these new drugs that are being developed if we rely on PFS overall survival, the sort of traditional clinical endpoints. So that’s sort of the general push is to make it so that effective drugs can get to patients faster.
Now with that, of course, comes a lot of risks and that’s sort of the balance, the conversation. That’s why this is something that’s so fun to cover. There have been sort of cautionary tales that FDA definitely brings up about drugs having really good early responses in MRD, or even in PFS I believe there’s other early endpoints and then having either a neutral or a detrimental effect on overall survival down the road. So that’s sort of the balance that FDA is always trying to strike here is not wanting to keep patients who… Especially in myeloma, let’s say hypothetically a patient goes through all of the available therapies and has no next step. That’s I think the… If I remember correctly about the myeloma one, and that was a story I wrote a while ago. So I might not be remembering all the details perfectly correctly.
But in that case, that’s where you want to be able to get a new therapy out to patients quickly if they work and if they’re effective, but of course, you also want to be really careful. So that’s sort of the broader narrative there. But this specific story was about the ctMoniTR project. And this kind of goes back to MRD in multiple myeloma as well, is that to get to the point where FDA or ODAC and FDA feel comfortable approving drugs or granting accelerated approval for drugs in multiple myeloma using MRD as the primary endpoint, to get there, it was over a decade-long… Project is maybe a strong word, but effort. It started out quite disjointed. There definitely were inefficiencies because it wasn’t sort of this unified plan to do this. It was driven largely by one person at Sylvester who felt confident that this was the way to go, and he sort of just pushed and the science panned out and it is an effective endpoint. Early endpoint not to be confused with surrogate endpoint.
And so basically Friends saw this in MRD and said, we don’t want this to be the case in ctDNA for solid cancers because that’s a waste of everyone’s time. And again, not to say that MRD, that was an amazing Herculean effort, everybody at the ODAC… I think three different ODAC members called it Herculean. It was only laudable, but there were definitely spots where we could learn to do better, and that’s what Friends is trying to do. And so the impetus for this story specifically is that they had a new readout of some of their data, one of their projects, that demonstrated that decreases in circulating tumor DNA after the initiation of treatment and it was immunotherapy or chemotherapy, I believe, are associated with improved overall survival in patients with non-small cell lung cancer, like you said, Paul.
It’s very preliminary. It’s not like this is proof that ctDNA works. We’re not there yet. But basically it’s another promising signal that ctDNA is, like MRD, something that we can use for early or quicker outputs of clinical trials in certain cases. So yeah, it was a really fun story. It’s fascinating. Very statistics-heavy, which is not how my brain works, but definitely something I want to keep an eye on too as ctDNA continues to develop as an endpoint.
Paul Goldberg: Yeah, no, this is fascinating. I’m glad we’re on this story and that’s why it was important to get that on the cover. It takes a while to get through it though, or to get to it because they’re flooding the zone, as you may notice. They’re actually not flooding it quite as much. Where shall we go next? Should we talk about… What’s the other story you’d like to discuss?
Jacquelyn Cobb: I think we should talk about your story and then maybe we can pop back over to GRAIL briefly. But I think the next story should be about Kyle Walsh, the-
Paul Goldberg: Oh, yeah. Very interesting. I knew him because he wrote a piece for The Cancer letter some years ago, like three years ago, about this series of stories in the Philadelphia Enquirer that basically said that AstroTurf from the baseball stadium… I believe the baseball team was called the Phillies. Is that correct?
Jacquelyn Cobb: I don’t remember. I’d have to look it up, but keep going.
Paul Goldberg: Please look it up because this is really bad because my knowledge of baseball is dwarfed by my knowledge of football, which I know absolutely nothing about.
Jacquelyn Cobb: I’m with you, unfortunately.
Paul Goldberg: Yeah, yeah. So anyway. So there was this discussion that AstroTurf causes glioblastoma and is associated rather with glioblastoma or maybe causes… I don’t know what Philadelphia Enquirer said, but it was clearly not something that Kyle wanted said and Henry Friedman as well from Duke. So these two guys are Duke. So he was just named director of the NIH Institute of Environmental Health Sciences. It’s very interesting, because I mean, this is a nomination that can be political and is usually. Sometimes it’s not, but in this case it clearly is. Kyle is a friend of JD Vance’s from Yale. They were both guys from Ohio at Yale, and they went to watch various sporting events together, and for a while… Actually, well, JD Vance at the wedding of Kyle’s, and for a while he was renting a room in San Francisco from Kyle and his wife, who is a pediatric dermatologist in Durham at the Duke Health System.
So, it’s a very interesting question, because I mean, this is a political appointment. Now, the fact that these two guys are friends, and I mean we’re talking best friends pretty much, well, is not a problem for anybody. I think the answer is no. It’s actually kind of good that here is an NIH Institute that has political juice behind it. If I were working for national… Well, if I were working for NIH I would say that’s probably a good thing. Now, there’s a really funny story with this. In March… It’s a much greater detail than the story itself. JD Vance and his wife and Kyle and his wife went to the Kennedy Center and were squarely booed. I have a link in the story where you can just watch them looking awkwardly, kind of like, “What did I get myself into?” I’m sure JD Vance knew, but Kyle probably understood it less acutely until that moment, and now he kind of does or should.
But he was booed. He understands that there’s a Newtonian aspect of what’s being done and with the flooding of the zone and so forth, and he’s in some ways a part of it, but it’s also an opportunity for him to do something good and for good things to happen. So in a way, maybe it could be I cautiously say an inflection point in all of this, having somebody there, and… I mean, I knew him before any of this happened. I didn’t know anything about JD Vance and him being besties.
Jacquelyn Cobb: But now you do.
Paul Goldberg: Now I do and now so does everybody else in science, and they stuck that story in there, all that detail about them being friends and about their kids being friends and their wives being friends, family vacation together kind of friends. So is that bad that that relationship exists? I don’t know. Probably not. Actually, I think it’s neutral to good somewhere in there.
Jacquelyn Cobb: Yeah. Yeah, definitely. And we’ll find out. We’ll see how things go as he continues.
Paul Goldberg: I mean, look, I called a bunch of people whom I respect a lot, and they all said, “Yeah, this guy’s good. He’s not traditionally in the… He’s an epidemiologist, an expert in glioblastomas, he’s been involved in a bunch of clinical trials, but he’s not really an environmental scientist in the traditional way.” Who’s to say that that’s not the right kind of person to run National Institute of Environmental? Plus, he’s a cancer guy for [inaudible 00:15:43]. The possibilities for NCI and for researchers at NCI to work with the National Institute of Environmental Health Sciences are enormous. So yeah, it’s nice. I think I would view this right now as a cautiously good news.
Jacquelyn Cobb: Awesome. Very nice. I feel like we’ve had a few weeks of that type of thing, so that’s really nice.
Paul Goldberg: Where I come from, we say Keinehora. May there not be an evil eye on this one. So I don’t know if The Cancer letter believes in the evil eye, but don’t say anything good. I just have, so that’s a bad thing. Keinehora.
Jacquelyn Cobb: That’s my version—knocking on wood.
Paul Goldberg: Can you say Keinehora?
Jacquelyn Cobb: I don’t think I want to try.
Paul Goldberg: Okay.
Jacquelyn Cobb: Yeah, I took Latin in high school for that reason so that I didn’t…
Paul Goldberg: That’s not Latin.
Jacquelyn Cobb: Well, no, exactly. That’s what I’m saying. I really have avoided speaking languages out loud since seventh grade, so I’m not going to do it on YouTube.
Paul Goldberg: Well, anyway.
Jacquelyn Cobb: Okay. Well, I will take us through just sort of the last bit that we’re going to talk about today. I don’t anticipate talking too much about this today because it’s still developing, but last week, the PATHFINDER II study results came out, and that is the most recent and most extensive study out of GRAIL of their Multi-Cancer Detection Test called Galleri, and they had a really strong media push about this. So I definitely wanted to just cover it because that’s sort of something that we’ve covered in the past, and I think is… If you look at the other coverage, I don’t think… I think we’re somewhat unique in the way that we cover MCED. So definitely wanted to get our perspective out there. But this is something that I’ll be continuing to cover. So this is not at all complete.
But the recent results from the PATHFINDER II study showed that the addition of GRAIL’s MCD test to standard screening led to a seven-fold increase in cancers detected within a year. And yeah, I mean, there’s a lot to sort of talk about with that. I think it’s really interesting that this is sort of the result that they’re coming out with. And importantly, this trial, according to GRAIL, is a registrational trial. So this is what they’re going to be taking to FDA to try to get the pre-market approval. So it’s a type of approval that is for devices. Yeah, I mean, I’m going to be following that closely. Can’t wait to hear what FDA has to say about it.
But obviously in the past we’ve talked about how with all screening tests, but specifically with a multi-cancer screening test, it is quite tricky to actually measure or validate the clinical impact, benefit or harm depending on what the reality is, and it seems that the MCD field in general is understandably hesitant to do what is necessary to prove that, which is do a trial with a mortality endpoint. And again, understandably hesitant because that kind of trial would take lots of time and lots of money. So it makes sense. But I think speaking to experts and stuff, this has been an ongoing concern, is that without that mortality endpoint, it’s really hard to know for sure if these tests are introducing benefit or harm to the public.
So, yeah, this is something that we’re going to be talking more about. I think the fact that they had a sevenfold increase in cancers detected, I don’t know… Yeah, okay. We don’t know. And that’s what’s so tricky is that public intuition and human intuition in this case is, of course, we want to catch more cancers, we want to catch more cancers earlier, but we just don’t know if that’s actually beneficial to people yet. Yeah, I mean, that’s at least my understanding of it as someone who’s covered this. I definitely, like I said, plan on reporting more and diving into this in more detail, going to get some expert’s opinion on the PATHFINDER II results, excuse me, and hear more about it. But yeah, just a day one story to keep up with the news.
Paul Goldberg: Well, that one is a really interesting story because it’s just a huge number of really profound questions, and NCI is trying to set up a study, its study, the Vanguard, to address these questions. And there are three tests, and Galleri isn’t one of them.
Jacquelyn Cobb: I think there’s only two, if I remember correctly.
Paul Goldberg: There are two tests and Galleri isn’t one of them. Let me repeat, Galleri isn’t one of them. Obviously they’re trying to get FDA to say what it is that they’re trying to do. It would kind of possibly make sense to focus on one disease or perhaps one where there’s no existing tests, like pancreatic cancer, or lung cancer where there are tests, but this could be a good one. Who knows? It’s a developing field, and the thing to do is not to prejudge any of it and to just report it, which we are doing. Thank you. And I’m somewhat involved in that as well. But it’s interesting, as I edited that story, I looked for the word early. E. Capital E. It’s not, Multi-Cancer Early Detection Test, but Detection Test, MCD, and that’s the NCI preferred language, and we accept that because we don’t really know whether these things are being found early or not early. So it’s kind of becomes kind of commercial speech, and that’s not going to happen here. So it’s a language that’s not always scientific.
Jacquelyn Cobb: Yeah. Yeah, I mean, that definitely is, like you said, part of the sort of marketing angle, the way that they’re selling it is that it’s… And not even just selling it literally, but even the way the press release for the PATHFINDER II results, it’s very much focused on this early detection, and we don’t know for sure, like you’re saying, that that’s actually what they’re doing.
Paul Goldberg: Yeah, we don’t know what the FDA’s thinking is on this.
Jacquelyn Cobb: Well, can I just… I mean-
Paul Goldberg: Please, please.
Jacquelyn Cobb: So, this is something that I’m going to be paying attention to, so I’ll just say it. So, basically whenever the last time I covered this was, I think it was last year, 2024, I had covered a class action lawsuit that was brought against GRAIL, and its former parent company, Illumina, and I didn’t get too much into that in the story because that case has been… The judge granted the motion to dismiss that complaint for failure to state a claim, but with leave to amend. So basically, to my understanding… Again, not a lawyer, not understanding of law very generally, but it’s some technicality with how the case was presented.
Paul Goldberg: This week, we’re going to have a story that will say whether the case has been refiled and it was dismissed without prejudice, which means it can be refiled. And has it been refiled? We’ll find out. So it’s an interesting question about insider information traveling-
Jacquelyn Cobb: Well, but the reason I brought that up was because in that case, part of it was that FDA had directly told GRAIL, I don’t know if it was part of Illumina at that point, but had told GRAIL that the studies that they had planned for approval were, I think, quote, “wholly insufficient.” And so that is sort of my main question is I would love to know what FDA is thinking about this in a more substantial verified way. But I think that that’s… I mean, even the ODAC meeting that we… Or it wasn’t ODAC. Actually, I’m sorry. It was a different advisory committee meeting about MCDs. I think that was also 2024 in April where FDA seemed to understand, or some members of FDA seem to understand the importance of demonstrating clinical benefit rather than just assay validity. So yeah, definitely a lot to talk about, lot to report on, and there will be more stories coming.
Paul Goldberg: There will be more, and I think NCI trial is an important part of that story, and it should be told, and we’ll continue. And also, let’s not forget that FDA is not static, especially right now. And like it or not, they may be changing their minds in different ways. So who knows? I most certainly do not. Anyway.
Jacquelyn Cobb: Long talk today, long conversation.
Paul Goldberg: Yeah. Very interesting. Well, I’m glad we had this little talk, and this is an excellent time to be a journalist.
Jacquelyn Cobb: Yes, yes. For those of you who don’t know, I’m glad we’ve had this little talk, is Paul’s new catchphrase every time he hangs up the phone with me. So, it’s very fun. I’m loving it. Glad we had the little talk, Paul. See you next week.
Paul Goldberg: Bye-bye.
Jacquelyn Cobb: Thank you for joining us on The Cancer Letter Podcast, where we explore the stories shaping the future of oncology. For more in-depth reporting and analysis, visit us at cancerletter.com with over 200 site licensed subscriptions, you may already have access through your workplace. If you found this episode valuable, don’t forget to subscribe, rate and share together. We’ll keep the conversation going.
Paul Goldberg: Until next time, stay informed, stay engaged, and thank you for listening.