After having treated over 200,000 COVID cases over two years—more than any health system in the U.S.—Northwell Health once again finds itself in the center of the storm as cases of the omicron variant escalate in New York State.
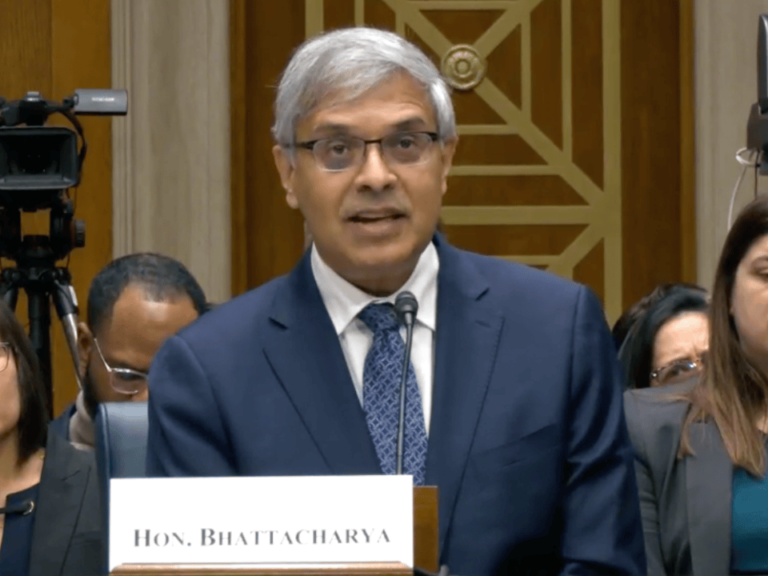
How does omicron differ from previous variants? How has preparation for its onslaught been informed by the past two years of the pandemic? How will cancer services be affected? The Cancer Letter posed these questions to Richard Barakat, physician-in-chief and director of Northwell Health Cancer Institute and the Edward and Carol Miller Distinguished Chair in Cancer.
A conversation of this sort should begin with numbers:
- Today, on Jan. 5, 2021, Northwell is treating 1,500 inpatients with COVID at its 23 hospitals.
- Of that number, 20% are being treated for other illnesses, and were incidentally found to have COVID. Nearly all of these patients are asymptomatic. The other 80%—1,200 patients—are admitted to the Northwell hospitals for COVID.
- Of the patients treated for COVID, about 9% are in the intensive care units, and about half of them were intubated. By way of comparison, in the first wave, about 20% of patients ended up in ICUs, and a much higher proportion of these patients required intubation.
- The background positivity rate in the communities Northwell serves is at about 25%. However, system-wide, fewer than 3% of Northwell’s 77,000 employees are out on sick leave.
“We’re definitely seeing our highest positivity rate ever. Nassau County, where our main campus is located, has over 25% positivity rate in testing,” Barakat said to The Cancer Letter. “So, we’re seeing a tremendous number of infections. What we’re seeing is an uptick in hospitalizations now. We are, fortunately, not seeing as many ICU admissions as we did last time. So, we are starting to pivot, like we did last time during that wave.”
Since vaccination of the workforce is required, most are either asymptomatic or experiencing mild symptoms—and most can return to work within five days with or without a negative test, if they haven’t had fevers over 72 consecutive hours, per new guidelines from the Centers for Disease Control and Prevention.
All cancer services—including early detection—continue to be offered, but new elective surgeries will not be scheduled in January. (Those that had been scheduled in December will proceed.)
Also, the health system is once again shifting to telemedicine, and, as earlier in the pandemic, patients can no longer be accompanied to their appointments.
Northwell’s COVID experience has been documented in a book co-authored by the health system’s President and CEO Michael J. Dowling, and in an upcoming documentary by National Geographic.
Barakat spoke with Paul Goldberg, editor and publisher of The Cancer Letter.
Paul Goldberg: Well, Dr. Barakat, first of all, thank you so much for agreeing to talk with me, and happy new year.
Richard Barakat: Happy new year to you, too.
Last time we talked about COVID was in July 2020, and you were just opening up again after being hit. Now there’s another peak coming, and you’re right in the middle of it, or the beginning of it, I should say. So, how does this look different from that?
RB: Well, first of all, thank you, Paul. We’re definitely seeing our highest positivity rate ever. Nassau County, where our main campus is located, has over 25% positivity rate in testing.
So, we’re seeing a tremendous number of infections. This is resulting in an uptick in hospitalizations. We are not seeing a significant increase in ICU admissions, as we did with the last wave, which reflects the propensity of omicron to affect the upper aerodigestive system while sparing the lungs, for the most part. So, that’s something that’s different.
Vaccination has played a key role in decreasing the severity of disease.
We are starting to see cancer patients who are getting treatment that are testing positive. We test all of our patients before undergoing chemotherapy or when therapy is being changed. Many of those who turn out to be positive are asymptomatic if they’ve been vaccinated, but some are symptomatic.
We are, fortunately, not seeing as many ICU admissions as we did last time, significantly less ICU admissions, but we are seeing an uptick in hospitalizations. So, we are starting to load-balance, like we did last time during the last wave. New elective surgeries will not be scheduled in January, but can be scheduled in February.
The health system is once again shifting to telemedicine, and, as in the earlier days of the pandemic, patients can no longer be accompanied to their appointments.
What about your own labor force? What’s the positivity rate?
RB: Well, with a 25% background positivity rate in the community, our labor force is definitely being affected. System-wide, however, less than 3% of our more than 77,000 fully vaccinated team members are out on sick leave.
This has not impacted patient care, as we are able to cover their roles through re-deployment of staff and use of our own internal temporary staffing agency.
Fortunately, the effect on the cancer institute has been very manageable. The rules based on CDC guidance have changed, and currently we are working in a contingency mode.
For those employees that are exposed to someone with COVID, if they’re asymptomatic, they continue to work and undergo COVID testing on day five. For the employees that test positive, we keep them out for five days now, and if they have not had fever for 72 hours or are only mildly symptomatic and improving, we allow them to come back to work with or without testing.
Every single person working in patient-facing areas must wear an N95 surgical mask that’s fitted to make sure that it functions properly, and a face shield. So, we are trying to get as many of our frontline workers back to work as soon as possible and that’s ongoing.
The five-day period definitely gives us more flexibility. If you remember, not too long ago, the CDC recommendations were 10 days, and that really would impact the workforce.
So, we are seeing infections increasing amongst staff, but the fact that we can get the affected and exposed staff back to work sooner, is a good thing.
What can you say about the effectiveness of vaccines? What are the percentages of people who are vaccinated?
RB: Everyone working in the Northwell healthcare system is vaccinated in compliance with the New York State mandate governing health care workers.
What we’re trying to do now is move from defining being fully vaccinated as having received two doses of either Pfizer or Moderna, to really meaning that you should receive the booster as well, because we know that the effect of the vaccine starts to wane after several months.
During the current omicron wave, vaccinated patients have a fivefold lower risk of being infected with COVID than the unvaccinated and a 31-fold reduction in those who are boosted. So, we really want every one of our team members to get boosted for their safety and the safety of our patients.
The question moving forward will be, and I know studies are ongoing in Israel, whether you need an additional (fourth) dose, but patients who have been fully vaccinated and boosted, are not getting sick with omicron unless they have underlying conditions.
Now, what we’re seeing is really a dramatic rise in COVID cases. If you look across the United States, it’s just astronomical, the number of infections. We’ve never seen that level before.
We learned a lot from that first wave, and I think we are well prepared to increase our staff. We are also prepared to bring in outside staff as needed to keep operations running.
So, we want to be careful this time. We are definitely seeing more COVID admissions to our hospitals. As of the beginning of January, we have instituted load-balancing. Currently, we are not allowing any more booking of elective surgery for January although those cases already booked in December are being allowed to proceed and we are currently allowing elective surgical cases to be booked for February.
We’re trying to keep the elective surgical volume in January when we expect the current wave to peak to be about 50% to 75% of the level that it normally is, and that’s just because as you increase the number of admissions for COVID, you need those beds available for those patients.
We categorize our surgical cases by tiers. Surgery that needs to be done immediately to avoid patient harm are Tier 4. Those are emergent cases and are ongoing. Cancer cases are considered Tier 3. Those are cases that cannot safely wait for a month to be performed so we certainly are doing our cancer cases. For completeness, I’ll mention that Tier 2 cases can be delayed up to three months, while Tier 4 can be delayed up to six months.
One of the really great things about Northwell Health as a healthcare system is, we have 23 hospitals, and we can shift patients throughout the system with load-balancing. And I think it’s a model that’s been adopted by others. The New York State governor has asked all hospital systems in New York to do that now.
You have to look at what your ICU capacity is as the admissions increase, and if you start to take up ICU beds, you have to shift patients within the system and not outside of the system. So, we’re always monitoring that carefully, as well as closely tracking the number of admissions.
In terms of our patients receiving chemotherapy, we will pause treatment if they are symptomatic until they have recovered for at least a week. We have some asymptomatic patients that are tested at home for various reasons, and we also will pause on those until we determine how their COVID course is progressing. Since delta is also present, we can’t assume that they will have the milder symptoms associated with omicron.
We continue to treat patients receiving radiation, regardless of symptoms (depending on severity), but leave them until the end of the day and utilize full precautions (PPE, sterilization of rooms).
Right now, pretty much everybody I know is sitting around and hypothesizing: At what point do you think we will know what’s actually going on, how omicron is behaving? When will we know what we’re up against? Another week? Another two weeks?
RB: I think everybody expects that we’re going to hit the real peak probably by the end of January.
So, I think within the next few weeks we’ll know. And I think if we experience what they experienced in South Africa, very rapid onset, very large peak, and then a rapid decline, we’ll hopefully get through this by the end of January.
Is this the beginning of herd immunity? But I’m hypothesizing.
RB: I’m not an expert in virology, but I think it probably is. This is what you see with viral infections. A virus is an organism that wants to live, and if it kills the host, in this case human beings, it won’t be around long.
The first wave tends to be the most lethal.
And then, as the virus mutates, it mutates to a form that’s less virulent, but highly infectious. Although I don’t know this for a fact and I don’t have a crystal ball, I think this wave might lead to herd immunity.
We’re getting to the point where so many people are vaccinated and hopefully boosted in the United States. Others have, unfortunately, succumbed to the disease, and now so many are getting infected.
So, I think we are starting to look at herd immunity at some point in the near future. And the hope would be maybe next winter, you’re going to get a flu shot that’s combined with COVID. Maybe FLUVID, a combination of flu and a COVID vaccine.
What about cancer screenings? Are you interrupting that—mammograms, etc.?
RB: We are not. And we are really encouraging patients not to do that. As you know, when we spoke last year, based on patients not going for screening, the NCI modeling branch predicted in the next decade, 10,000 additional deaths from breast cancer and colon cancer.
The good news is we are keeping our ambulatory centers, including our ambulatory surgery centers, open. We aren’t canceling anything at this point. We are continuing to do screening, but we’re practicing safety measures, making sure that our patients are not symptomatic.
And for our staff, as I said, we have made tremendous efforts in acquiring PPE for the system, and all staff that are in patient-facing areas must wear N95 masks and face shields.
So, we do not intend to shut down our screening. Now, with some patients, that’s going to occur by choice. They will not want to come in. Patients know that we are encouraging them to proceed with their screening as they normally would.
What about PPE? Obviously, it’s not a problem anymore. It was before. How did you prepare? Do you have a big strategic supply?
RB: We do. We have a very large strategic supply. We have a very large warehouse, which procures equipment for the whole system. And that’s one of the advantages of a large integrated healthcare system, economies of scale, that allow us to procure a great deal of supplies in bulk.
And we are comfortable with our supply. We feel that we will have enough supply to handle even this major surge.
The other thing we’ve done is planned for surging our staff through our internal temporary staffing agency. In addition, being New York State’s largest private employer allows us to redeploy staff as needed throughout our system.
We learned a lot from that first wave, and I think we are well prepared to increase our staff. We are also prepared to bring in outside staff as needed to keep operations running.
What about financial losses? Last time we talked, in 2020, it wasn’t really clear what that would end up being for you. Did anything happen in 2021 that affected your bottom line, related to COVID? How do you control financial losses now with omicron?
RB: Well, I think we learned a lot. Clearly, we benefited from money that came from the CARES Act. We had to pivot a lot and change the way that we practice. There was a pause on surgery for a while. But based on some of the changes we made, some of the cost-cutting measures we undertook, we actually ended up the year in the black in 2021.
We did have a small positive margin, but again, we did benefit from federal funding. As you know, Northwell as a system took care of more COVID patients than anyone in the United States.
And again, we will do everything this year to make sure that we keep operations running efficiently. We are mindful of expenses. And some of the expenses have gone away, because people are not traveling as well, of the other things that improve the bottom line. So, I think we just have to be very, very careful and keep things running as best as we can.
Ultimately, at the end of the day, when you are cutting back on surgery and infusions and treatments, that’s going to affect the bottom line. But I think that this wave is different from last time.
We don’t have ICUs filled with patients. We don’t have as many people dying as we saw in the past. So, I think we are going to do everything to keep operations running as close to normal as possible.
Who are the patients who are in the hospitals now? Because last time around, it was people who were living in close quarters, which I guess describes a lot of New Yorkers. Who is it now? It was the underserved. Right now, I’m looking at whom I know who is sick, and it’s at least more than a dozen people, including a Cancer Letter reporter.
RB: Well, in some ways, it’s becoming the pandemic of the unvaccinated. So, clearly, we know that people that have been vaccinated have a five times lower risk of getting infected with omicron and those that have been boosted have about 35 times lower risk.
Unfortunately, it appears that patients with omicron have a three to five times higher reinfection rate than patients with delta.
So, it’s really, in a sense, a pandemic of the unvaccinated. The other factors that lead to degree of sickness are the classic things that we saw last time, the comorbid medical conditions, obesity, diabetes, immunocompromised state. And, of course, it differentially affects ethnic and minority populations.
But we’ve made a major effort to get vaccinations out into the community. It takes a lot of work. We have an outstanding community program where we have community engagement. We work with churches, synagogues, community centers to provide vaccines. We have a massive vaccine distribution effort.
And we really get out into the communities and do a lot of grassroots efforts to try to get those underserved populations vaccinated, and I think we’ve done quite well with that..
Well, community outreach and engagement is something cancer centers have done, or should be doing, well. But do you get any sense of who the vaccine resisters are in your area?
RB: It’s different for different individuals. Obviously, there’s a lot of discussion about political views and things like that. People have their own beliefs. The state mandated that all healthcare workers get vaccinated. We lost less than 2% of our team members due to vaccine hesitancy.
But we do have a very large system, so it didn’t affect our ability to care for patients. People have their reasons for not wanting to get vaccinated. We feel very strongly that vaccination is so important. But now we’ve got another push in our system, it’s not only initial vaccination.
As I mentioned, I think the new definition of fully vaccinated will be boosted as well, because we do know that immunity wanes after a while, and that especially with omicron, it’s extremely important to be boosted as well.
The other thing we’re trying to do that’s worth mentioning is primary prevention for our high-risk patients.
For our immunocompromised patients, there’s a new preventative therapy called Evusheld, which is a combination of the monoclonal antibodies tixagevimab plus cilgavimab which we are fortunate to be one of the sites that is going to be rolling this out.
You have to think from an operational standpoint how to make things safer. We realized that when we bring cancer patients to get an infusion of chemotherapy, we have them sitting and waiting inside the cancer center for a while, before going back for their infusion. So, we say, ‘Well, we shouldn’t be doing that.’
It’s two intramuscular injections given six months apart as prophylaxis. We currently have a limited supply of doses, and we’re going to start rolling it out to our high-risk patients including those undergoing stem cell transplant, CAR T-cell therapy, leukemia, lymphoma, multiple myeloma and others who may not mount an effective response to vaccination. Obviously, as it’s an IM injection, they have to have platelet counts above 20,000.
This agent is intended for pre-exposure prophylaxis and is not intended for those with COVID infection or known recent exposure. The agent is active against both the delta and omicron variants and reduces infection rates by 70-80%.
In terms of therapeutics, we are actually going to be prescribing the Pfizer drug Paxlovid, which recently received FDA emergency use authorization for the treatment of patients with mild to moderate COVID infection who are at high-risk for severe illness which of course includes cancer patients.
The use of Paxlovid in these patients within five days of symptom onset was associated with an 87% decrease in hospitalizations from COVID. It does have side effects and significant drug-drug interactions which clinicians need to be aware of.
The other drug that received EUA for high-risk patients is the Merck drug Molnupiravir, but it appears to be most effective if used within three days of symptoms and had a more modest reduction of 31% in admissions compared to placebo.
Finally, the monoclonal antibody Remdesivir can prevent progression to severe infection in high-risk patients with an 86% reduction in hospitalizations vs. placebo, but it needs to be given as a three-day infusion.
So, therapeutics continue to play an extremely important role in prevention and treatment of COVID in cancer patients.
And, of course, vaccine, vaccine, vaccine, vaccine.
Is there anything we forgot? Anything you’d like to mention?
RB: I think we just have to be vigilant. We learned from the first wave that you have to pivot. So, we are pivoting again. We are going to load-balance and increase the use of telehealth for patients who have routine follow-up appointments. You have to decrease the flow of traffic in the ambulatory setting as well as the hospitals.
I think you also have to pivot in terms of how you treat some patients. Again, there are often options for treating patients, where you might consider neoadjuvant therapy versus doing radical surgery right off the bat.
Dosing and scheduling modifications for chemotherapy infusions, such as switching to once-every-three-weeks chemotherapy versus giving weekly chemotherapy. Switching to oral agents that don’t require infusions in the hospital. These are changes that are relatively straightforward to implement.
You have to think from an operational standpoint how to make things safer. We realized that when we bring cancer patients to get an infusion of chemotherapy, we have them sitting and waiting inside the cancer center for a while, before going back for their infusion.
So, we say, “Well, we shouldn’t be doing that.” If they have a car, and of course in our area, they have the heating on in the car, let them wait outside until we call them. When they are brought in, they should be taken directly to the infusion center and start their infusion immediately. There’s no point in having people sitting around and waiting and increasing exposure.
We, unfortunately, have to, again, institute a policy of not allowing family members in the infusion center, which is, of course, upsetting. But communicating regularly with the family can help alleviate their anxiety.
But for the most part, we’ve decided that we have to stick with that because anything you can do to reduce the flow of traffic and avoid transmission of COVID is important. Even amongst our own staff, we’re encouraging distancing. We’re all wearing masks. Meetings are all mostly Teams or Zoom. We’ve seen this movie before, so we know the script quite well.
And speaking of seeing this movie, there’s an unbelievable documentary that was filmed in the first wave of the pandemic which has recently been released. It did have its premiere at the Beacon Theater in New York. It’s called The First Wave, and it documents the fight against COVID at Long Island Jewish Hospital, which was really the epicenter of the epicenter here in Queens.
It was filmed in March of 2020, and is an incredibly moving documentary about what happened during that first wave, and I strongly encourage readers to watch it. It’s well worth it. It’s currently streaming on Hulu.
So, that’s pretty much where we stand, exciting developments in therapeutics between Evusheld as prohylaxis as well the Pfizer drug Paxlovid for mild to moderate high-risk patients. And we’re hoping that this current wave finally gets us to herd immunity, between the vaccinated and patients who have natural immunity because they were infected.
Hopefully, this will signal the end of it, but I guess we just have to wait and see, Paul; right?
I guess I’m not hearing you’re being concerned about the system being overrun. It’s not going to happen? Or would you know it yet?
RB: Paul, we track this daily. It is a tremendous amount of work that’s being done to keep a very close eye on this. In fact, when you look at the curves that are published daily we’re seeing that hospitalizations are following what they did with the last wave. But where curves diverge is the ICU admissions, and that’s what’s really encouraging.
We are anticipating that the hospitalizations are going to continue to increase. So, we are completely aware of what’s going on. We are closely monitoring the number of admissions, closely monitoring the number of ICU admissions, closely monitoring the number of staff that are infected.
We are looking at every aspect of this and we are ready to shift, load-balance and transfer between our 23 hospitals as quickly as possible. We do not intend to get caught off-guard, and no, we don’t think we’re going to be overrun but are doing everything to prevent that.
Our COVID testing capacity is now 20,000 per day. We have the largest lab in the United States, and we do a tremendous amount of testing. We also staff multiple vaccine distribution sites.
We are doing everything possible to make sure that we keep our patients and the communities we serve safe.
Well, thank you so much for talking with me.
RB: You’re welcome, Paul.