This story is part of The Cancer Letter’s ongoing coverage of COVID-19’s impact on oncology. A full list of our coverage, as well as the latest meeting cancellations, is available here.
Preparing for a surge in COVID-19 cases this week, the Johns Hopkins health system is relying on the recently-activated Johns Hopkins Medicine Incident Command Center to prioritize the institution’s patient care and research functions and coordinate the opening of testing tents and drive-through testing sites.
“As you might imagine, cancer care providers, researchers, trainees, and support staff are working intensely at the moment through Incident Command Center structures to ensure the best care for cancer patients through the expected surge in COVID-19,” William G. Nelson, director of Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins and professor of oncology, said to The Cancer Letter.
“My advice to other cancer centers is to activate hospital/health system emergency preparedness capabilities, such as command centers, and to work with public health authorities, other cancer centers, and health systems to share insights and implement best practices as all of us confront a massive surge in COVID-19,” Nelson said.
Nelson spoke with Paul Goldberg, editor and publisher of The Cancer Letter, on Sunday, March 15.
Paul Goldberg: Thanks for agreeing to talk with me. I am sure you are insanely busy dealing with this. What are we up against?
William Nelson: You are right, cancer centers are busy implementing a wide range of tactics in order to provide care for cancer patients with and without COVID-19, to ensure health and safety of employees, staff, and trainees, and to prioritize and preserve essential research capabilities.
How are you managing this?
WN: For clinical care of cancer patients, there will be increasing use of telephone and telemedicine interactions when treatment infusions, physical examinations, and procedures in the ambulatory setting are not felt to be absolutely necessary.
Intensive treatments/procedures, such as bone marrow transplants for sickle cell disorder, that can be delayed will be delayed.
Patient/family entry into treatment facilities will be restricted to points where screening for COVID-19 symptoms can occur. Family members accompanying outpatients of visiting inpatients will be limited to one, and all visitors will be subjected to screening.
As much as possible, patients are being screened by phone before essential ambulatory visits, such as for treatment infusions.
An algorithm is used for patients with symptoms compatible with COVID-19 that should secure rapid intervention (including isolation while needed) for those with neutropenia or who are on treatment with immuno-oncology drugs who may require urgent care or hospital admission.
Testing of symptomatic patients, including cancer patients, for COVID-19 is ongoing, using an in-house test at the moment.
Testing tents and drive-through testing sites are or will be coming on-line at all of our cancer treatment sites. Increased availability of testing over the coming days will be very helpful.
Laboratory research will be dialed down significantly, with essential needs, including welfare of laboratory animals, upkeep of critical instrumentation, etc., to be managed by a reduced number of people on-site.
Work at home has already been encouraged. There will be no visitors allowed in laboratory research facilities.
Clinical research will be similarly attenuated with new accruals to existing trials allowed only when medically necessary (for example, our bone marrow transplants are done as part of clinical studies).
Also, it’s unlikely that new clinical trials will be launched until the pace of the SARS-CoV-2 epidemic is better understood.
Finally, as you might imagine, cancer care providers, researchers, trainees, and support staff are working intensely at the moment through Incident Command Center structures to ensure the best care for cancer patients through the expected surge in COVID-19.
When and how did you set up the command structure?
WN: My memory is that the Johns Hopkins Medicine Incident Command Center was activated at the end of February.
We have had dedicated working groups of cancer center personnel focused separately on clinical care, laboratory research, clinical research, and training/human resources since around that time.
These worked as part of the JHM Incident Command Center until we activated our formal command center last week. Our command center rolls up to the JHM Center, enduring coordination of all functions: physicians, nurses, security, facilities, supply, etc.
What kind of in-house tests are you using? Were they on the shelf to begin with, or did you have to develop and manufacture them in a hurry? What can you say about the logistics and economics of that?
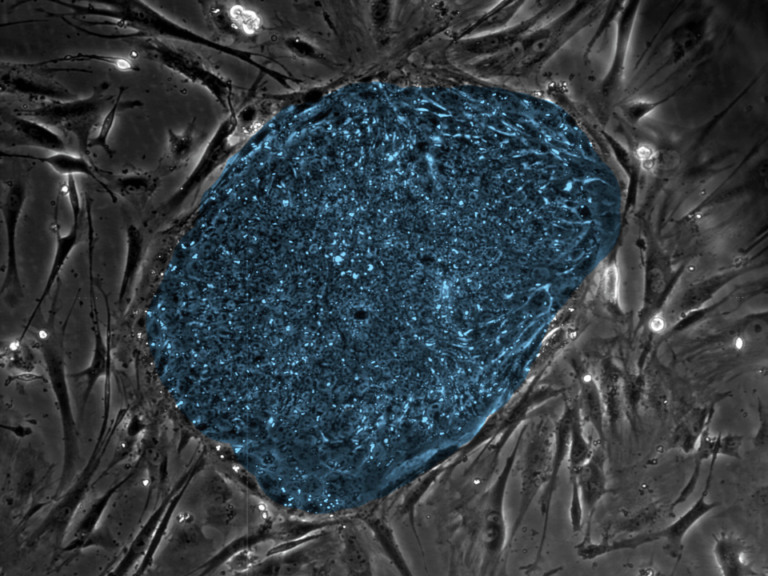
WN: Our Laboratory Medicine team created an assay compliant with the FDA Emergency Use Authorization, deployed last week and now scaling up rapidly. As commercial tests become available, I suspect they will also be used. I have no clue as to the economics.
As a scientist, what can you tell me about the way the virus is behaving? Does it behave similarly to the Coxsackievirus, for example? Can you prognosticate about what we are in for? How many cases? How long?
My advice to other cancer centers is to activate hospital/health system emergency preparedness capabilities, such as command centers, and to work with public health authorities, other cancer centers, and health systems.
WN: I think that there are many uncertainties related to SARS-CoV-2, including its mechanisms of pathogenesis, whether it will exhibit some sort of seasonality, what might be the nature of protective immunity (including whether antibodies from convalescent serum could be used in an emergency setting), how effective available treatment (tocilizumab, remdesivir, etc.) might be, and how long it will take to discover and develop more effective interventions, whether full-on “social distancing” might attenuate the surge of cases threatening to swamp health systems, and whether a vaccine can be created to arrest future threats from this virus in coming years.
What’s your advice to your colleagues at other cancer centers?
WN: My advice to other cancer centers is to activate hospital/health system emergency preparedness capabilities, such as command centers, and to work with public health authorities, other cancer centers, and health systems to share insights and implement best practices as all of us confront a massive surge in COVID-19.