Honorable Sen. Harris and colleagues,
I write this letter to you as an advocate for women with malignant uterine soft tissue tumors—and to commend you on the introduction of The Uterine Fibroids Research and Education Act in the United States Congress.
I, and on behalf of my late wife, Dr. Amy Josephine Reed, represent the interests of many thousands of women with uterine soft tissue sarcoma tumors in the U.S. and abroad. It is my duty as an American physician and public health advocate to inform you and the United States Senate of a critical women’s health hazard, which your bill can directly address and help eliminate in the United States.
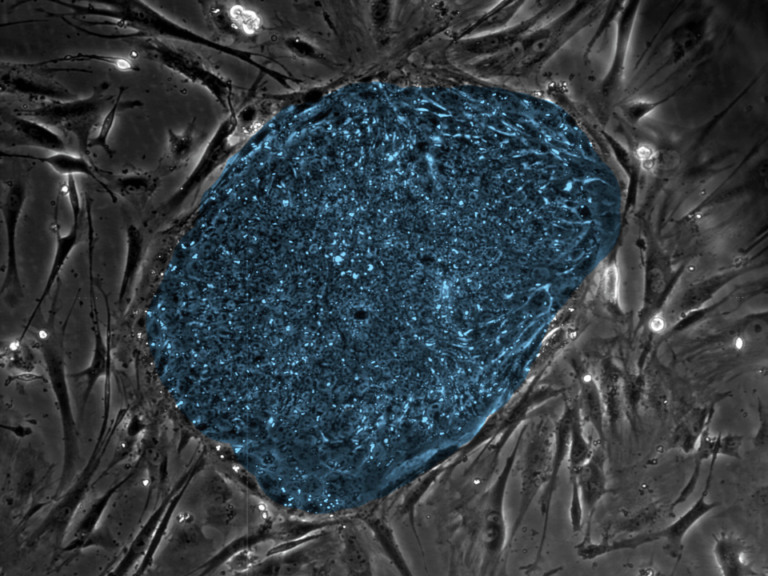
As you may know, soft tissue sarcomas of the uterus are dangerous malignant tumors, which masquerade as fibroid tumors in most affected women. Frequently, these uterine sarcomas are only diagnosed after uterine surgeries for what are assumed to be symptomatic benign uterine fibroid tumors. These uterine surgeries are the so-called myomectomy or “hyster-ectomy” operations offered to millions of women, annually, by benign gynecologists across the U.S., and worldwide.
Perhaps one of the most important aspects of Dr. Amy Reed’s advocacy over the years was related to the recognition that a large majority of the women we advocated for have uterine sarcomas, which are diagnosed only after their surgeries for uterine fibroid tumors—assumed benign, preoperatively. This is a dangerous and problematic fact in contemporary gynecology, as these tumors are, literally, all missed uterine cancer diagnoses.
To compound the problem, most benign gynecologists in the U.S., and abroad, disrupt and fragment fibroid tumors inside women’s abdominal cavities in a standardized process known as morcellation. The practice of morcellation, be it manual or mechanical, is routinely undertaken in order to extract enlarged uterine tumors through as small skin incisions as is possible—for reasons of cosmesis and convenience to patient and doctor.
But, when a uterine soft tissue sarcoma diagnosis is missed by American gynecologists, and the tumor is assumed to be a benign fibroid tumor, its surgical disintegration (i.e., morcellation) inside the woman’s body cavity causes the spread and upstaging of the missed cancer. In other words, the very surgery performed on these women’s uteri becomes an iatrogenic cancer mortality risk.
It is a verifiable fact in gynecology that the routine iatrogenic upstaging of missed uterine sarcomas has caused irreparable catastrophic harm to the lives of many women, whose sarcomas were upstaged and become incurable. The sad fact is that this hazard in women’s health persists to this day.
Unfortunately, as you might know, most sarcomas are resistant to chemotherapy. Thus, it is an established medical fact that the best chance of curing sarcoma tumors and prolonging the patient’s life is en bloc resection of the tumor with good surgical margins—and without in situ tumor disruption/morcellation, to prevent spread of the sarcoma. In order to do so, it is critical for these malignant tumors to be preoperatively identified, so as to avoid morcellating them.
This oncological danger of morcellation in the surgical treatment of uterine fibroid tumors by benign gynecologists came into full public light in 2013 through 2017. This, following a series of high-profile articles about the harm done to Dr. Amy J. Reed, and many other women, by minimally invasive gynecological surgery involving morcellation of the uterus.
The Wall Street Journal, The Cancer Letter, The Boston Globe, The Philadelphia Inquirer and The New York Times, all published series of articles informing the public and regulators of this danger in minimally invasive gynecology. At that time, FDA determined that nearly one out of every 200-400 women with symptomatic fibroid tumors requiring uterine surgery by a gynecologist, carries a sarcoma tumor, most assumed benign preoperatively.
You might already know that uterine fibroid tumors are the only prevalent tumors in the human body, which are routinely subjected to non-oncological surgical resections involving morcellation of the tumor—this, while almost none of these tumors undergo pre- or intraoperative tissue biopsy to establish a “reasonable assurance of benignity” using tissue histopathology. This failure to perform tissue biopsies on a highly prevalent tumor type with malignant potential, which is routinely assumed to be benign and undergoes in situ fragmentation, is unique to gynecology.
That is, uterine fibroid tumors are the only potentially malignant tumors in the human body that are not histologically assessed to rule out cancer, before the general gynecologist proceeds with a non-oncological operation with a high likelihood of spreading and upstaging cancer. This is a serious danger in the care of American women with uterine fibroid tumors—and it is potentially catastrophic to the minority, one in 200-400, subset of women whose missed sarcomas are subsequently spread and upstaged by morcellation in the course of “minimally invasive” operations on the uterus.
But really, the root cause of the problem I am now bringing to your attention is the gynecological “assumption of benignity” about uterine fibroid tumors. Though it is true that the majority of these fibroid tumors are benign leiomyomas, any reasonable physician, scientist or citizen would agree that these tumors cannot be assumed benign, because one in 200-400 are not benign! And, because, when such an incorrect assumption is made by American gynecologists, the lives of the minority subset of women whose cancers are missed, and then labeled “occult” for purely medico-legal reasons, are devastated by their surgery for benign fibroids.
It is a sobering fact to note that, with over 500,000 of these uterine operations performed in the U.S. annually, a one in 200-400 subset at risk is no small number of women in mortal harm’s way.
The most difficult problem for us to reconcile, one which your bill in the U.S. Congress can effectively resolve, is the question of why American gynecologists almost never utilize the well-established biopsy technique known as Core Needle Biopsy (CNB) to assess fibroid tumors and rule out a malignancy, before proceeding with a “benign” uterine resection operation.
After all, the fact that the majority of these tumors are benign, is totally insufficient justification for ignoring the potential catastrophic miss of uterine sarcoma diagnoses in one out of 200-400 women undergoing uterine surgery for fibroids tumors. Especially, when the operation offered by benign gynecologists, itself, devastates these women’s lives by exposing them to the iatrogenic risk of cancer upstaging.
Over the past seven years, Dr. Reed and I routinely queried many gynecologists and their professional associations about why standard CNB techniques are not utilized in the pre- or intra-operative evaluation of uterine fibroid tumors—in order that a “reasonable assurance of benignity” be established by the gynecologist. The answers we received from gynecological surgeons and their professional organizations have been unsatisfactory and—we recognize—baseless, without any real scientific merit.
That is, the position of most gynecologists in the U.S. and abroad is that CNB is insufficiently sensitive for detection of uterine sarcomas. We know this assertion to be false and primarily driven by the industry’s need to sustain its efficient economic status quo—not by established science or adequate medical ethical reasoning. In fact, the vast majority of other surgical specialties rely on CNB to diagnose many varieties of soft tissue sarcomas when confronted with tumors of unknown significance. Moreover, the scant case series we have found in the pathology literature focused on CNB for diagnosis of uterine sarcomas, suggests that these malignancies can be distinguished well from benign leiomyomas with reasonable sensitivity and specificity.
But, because the position/prejudice of experts within gynecological societies is against use of CNB for preoperative evaluation of uterine fibroid tumors, the “assumption of benignity” about uterine fibroid tumors, without any pre- or intraoperative biopsy, has become a standard approach by many American gynecologists. This fact has created and sustained a dangerous and systemic iatrogenic mortality risk to the one in 200-400 American women, whose uterine sarcoma diagnoses are being missed routinely by general gynecologists.
Through clear-sighted scientific reasoning and investigation guided by your proposed Uterine Fibroid Research and Education Act, this danger to women can be eliminated. Here, I write to formally request that you and your colleagues in the U.S. Congress act to specifically authorize federal funds to scientifically determine the efficacy of CNB techniques in preoperatively ruling out the presence of occult uterine sarcomas in fibroid tumors.
Importantly, your bill recognizes that well over 500,000 uterine operations are performed by benign gynecologists in the U.S. annually for management of symptomatic uterine fibroid tumors. As you’ve also established, Black women are disproportionately affected by fibroid tumors. Additionally, the CDC previously determined that the rate of uterine sarcomas is higher in the Black population as compared to whites. Therefore, it stands to reason that Black women, whose symptomatic uterine fibroid tumors are assumed benign, are disproportionately affected by the dangers of morcellation in uterine surgeries, compared to white counterparts.
Sadly, one of the major frustrations Dr. Reed and I faced, was our relative inability to identify and reach the many Black women who are almost certainly affected by the problem described herein. I believe that this failure to reach women of color is caused by: 1) Inadequate access to health information by Black women and 2) Inadequate outreach and education on the part of the American gynecological establishment about the malignant potential of uterine fibroid tumors to women in general—and, even more so, to Black women.
It is a verifiable fact in gynecology that the routine iatrogenic upstaging of missed uterine sarcomas has caused irreparable catastrophic harm to the lives of many women, whose sarcomas were upstaged and become incurable.
These deficits must also be corrected using cogent federal regulation like the one you are now proposing. I know that with adequate community engagement and resources dedicated to health literacy, all women, and in particular women of color, can be educated to make informed and safe decisions regarding their symptomatic uterine fibroid tumors and their malignant potential.
Our mantra in raising awareness about the issue raised herein has been: Simply, that a majority of women and a medical specialty enjoy an economic or convenience benefit, is not sufficient justification to sacrifice the lives and safety of a minority subset of women by assuming all fibroid tumors to be benign pre-operatively.
We trust that you agree with the merit of this perspective.
Finally, you have likely noticed that in this letter, I have refrained from using the term “hyster-ectomy” to refer to the gynecological operation involving the removal of a woman’s uterus. Instead, I have focused on using the terms “uterine resection” or “uterine surgery.” I have done so in order to avoid use of a professionally accepted term, which is without a question offensive and misogynistic, when referring to removal of a woman’s uterus in gynecology.
In fact, the term “hyster-ectomy” is a vestige of a bygone era when medical men believed the uterus to be the source of hysteria in women. We, as a nation, ought to revise our professional jargon to make it more objectively correct and less derogatory to all subsets of people and problems. Because, as you know well, the precision of the words we use to describe our world’s problems, dangers and injustices shape the empathy and acuity of our systemic approach to resolving them. The word “hyster-ectomy” ought to be offensive to every woman in the U.S. Congress and to our society at large—help us, also, correct this lapse in gynecological language in your bill.
Summary of requests on behalf of women vis-à-vis The Uterine Fibroids Research and Education Act:
That your bill acknowledges the danger lurking in the assumption, by benign gynecologists, that all uterine fibroid tumors are benign without any “reasonable assurance of benignity” using well-established tissue biopsy techniques.
That your bill direct federal funding of research specifically dedicated to establishing the sensitivity and specificity of Core Needle Biopsy for identifying or ruling out, within a reasonable margin, soft tissue sarcomas masquerading as, or hiding in, fibroid tumors, pre- or intra-operatively—prior to exposing any more American women to non-oncological uterine resections involving morcellation.
That your bill calls for federally funded community outreach and engagement programs to inform and adequately evaluate Black women with symptomatic uterine fibroids, so that their sarcoma diagnoses are not missed.
That your bill refrains from the unrestrained use of the misogynistic term “hyster-ectomy” when referring to the gynecological operation, which can be more appropriately described as a uterine resection.
Here, I write to formally request that you and your colleagues in the U.S. Congress act to specifically authorize federal funds to scientifically determine the efficacy of CNB techniques in preoperatively ruling out the presence of occult uterine sarcomas in fibroid tumors.
Sen. Harris and colleagues, perhaps through your review of the press and scientific coverage of uterine morcellation, you will recognize the scope of the public health battle, which Dr. Amy Reed and many individual women and their families have been waging since 2013, to bring rationality and safety to the care of women with symptomatic uterine fibroid tumors.
Here, I write with Dr. Amy J. Reed’s spirit with me, to respectfully ask for your firm support on a policy level, so that you might help bring safety through the use of science and ethical reasoning/language to the management of symptomatic uterine fibroid tumor in women—and Black women, in particular, because they are almost certainly disproportionately affected by the problem I’ve detailed herein.
These tumors of the uterus we call “fibroids” cannot be assumed benign by American gynecologists—tissue biopsy is a well-established technique that provides a rational solution to a deadly hazard affecting women—unjustifiably ignored by American gynecologists.
Yours in friendship and with respect,
Hooman Noorchashm MD, PhD
For Amy J. Reed MD, PhD and the others.