The Roche-Syapse collaboration to develop analytics programs may enable health systems to measure the impact of precision therapies, said Damon Hostin, CEO of the Precision Medicine Alliance.
Hostin oversees the precision medicine partnership between two of the nation’s largest nonprofits—Dignity Health and Catholic Health Initiatives—and is in charge of integration of oncology and other clinical data programs between the health systems. The network describes itself as the largest community-based precision medicine program in the U.S.
“As important as the core technology is, it’s about bringing the ecosystem together. And Syapse has been effective in doing this on a common platform,” Hostin said to The Cancer Letter. “This is, I think, a sign of the [precision medicine] field maturing, where it’s being beholden to any of the economic measures that any intervention would be held to.
“Some of the benefits tend to be the amount or depth of information, the genetic markers, be it economic, and then the other dimension of it is looking at the total lifecycle or extending the episode of care so that we more fully understand the impact of the medicines or risks.”
Hostin spoke to Matthew Ong, a reporter with The Cancer Letter.
Matthew Ong: What does the Roche-Syapse collaboration mean for the Precision Medicine Alliance, and for your provider partners? How would this change the way your health systems do cancer care?
Damon Hostin: In an agreement like this, just to speak generally, because in the Precision Medicine Alliance, we use the Syapse system, we of course as a major health care provider use many of Roche’s products, but the agreement is more substantive that it’s bringing together groups that traditionally are unable to cooperate more fully because of a lack of data access and transparency in understanding effectiveness and cost effectiveness of therapeutics in particular.
So what really excited me about this is that there is such deep knowledge in healthcare economics as it relates to the use of advanced therapeutics, and we all know the cost to bear of these therapeutics.
Roche is really bringing a ground level understanding of that field to the ecosystem and looking to cooperate with it. So, every time we hear about risk potential for, let’s say, risk-based payments or anywhere in which quality is now becoming a determinant on the payer side of healthcare, Roche is actually bringing a very rare perspective to healthcare.
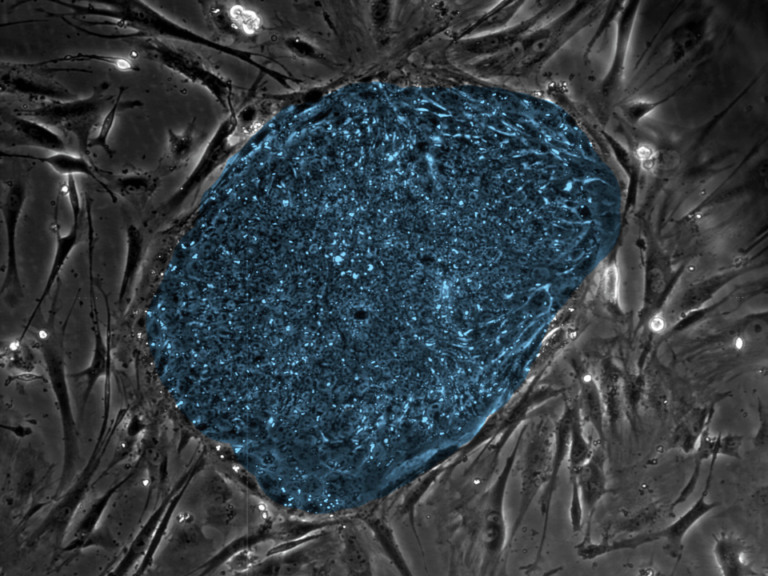
Now, Syapse is the platform that allows for the information to become relevant, and specifically, it is able to digitize the esoteric nature of cancer genetics, which is very difficult to put into a workable dataset alongside EMR data.
If you look at the two facets here, one of tumor biology and the other healthcare information, Syapse is able to bring back together. And I would say, the types of things that we’re going to look at is, “What is the value of any given modality outside of the drug itself? What was the cost of supportive care? Did it prevent adverse events? What is the overall burden of treatment and what is the differential of different interventions there within?”
So really giving a better resolution on the natural history of a patient so that we understand the costs, the risks, and can actually do comparisons across different product types. Knowing the patient better leads to better decisions.
I was very impressed that there is a willingness to be product agnostic, meaning the collaboration is a platform for understanding and it’s a window into the truth of the costs and risks, and that really hasn’t been done before with these types of partners.
And you’re saying this in the context of the four product programs that are going to be developed as a result of this collaboration.
DH: That’s right, this is all quite formative. When you ask how is it going to change what we do, of course this is all a little bit speculative, but you know, you always say if you can get everyone to the table to get a single source of truth about what we think or what is supposed in the clinics, well, we would have a much better handle on the practice of medicine.
For the first product, the concept of the “learning health system,” that is where if you’re not capturing and standardizing EMR data elements and putting them alongside the deep profiling of a patient, you really can’t make any conclusive findings around these populations.
What we’re looking for is it isn’t just the tumor profile, and it’s not just the elements of the EMR, it’s everything together. And so, if we’re standardizing language ontologies IT systems capture, that then allows us in a much more cohesive way to ask questions and get rid of the junk in, junk out—the problem that vexes health care economics.
And this is for the first pillar, which is focused on the curation and aggregation of real-world evidence, which enables practitioners look at ongoing treatment and outcomes data and get a well-rounded picture?
DH: It is, and that well-rounded picture is a broader view. So, understanding what is the cost of mitigation of side effects, for example. When a cancer drug is approved, there are generally two metrics: what percent of the population responded and what was the survival benefit.
And often it stops there. Physicians really don’t understand much more. But if a drug actually causes infections or anemia that needs to be managed in-patient, the whole concept is, that is also the cost of the drug; that is also the cost of the intervention, and rarely are these things in oncology any way fully captured.
In many ways, I think this borrows from the progress of volume to value as it relates to bundles and things like that. It’s really taking it quite seriously and understanding it and that learning, when, if these things are known, then a physician can balance the benefits and the risks across their choices of intervention.
But without this information, you’re just guessing and it’s anecdotal, and maybe publication-by-publication, but that’s not an efficient way for information to transfer through the system.
Right, and that sounds like it would tie into the third product program, which focuses on patient-reported outcomes.
DH: Yes, exactly. In some ways, I would say the first one is the umbrella of two of the others, so maybe we can walk through and they’ll piece together.
The “value-based era” is the economic impact that I was talking about, because we will be able to partner and put an overall cost of care beyond just the drug-gene-indication rubric of precision medicine.
So one of the things precision medicine really needs to do is stop being so exceptional and play by the same rules as any intervention in healthcare. Because of its novelty or its potential, it sort of has been given a bit of a pass for its early nascent years.
So this is, I think, a sign of the field maturing, where it’s being beholden to any of the economic measures that any intervention would be held to. In some ways, its exceptionalism, I believe, has hindered its greater uptake and potential, because no one ever measured this in the way that other things would be traditionally measured.
Some of these economic measures that you say are a sign of the field maturing, do they apply to the provider end as well as on the patient end? For the provider, it’s making sense of what to offer, and for the patient, it’s figuring out what is cost effective?
DH: Right, the full purview of it. Unfortunately, cancer tends to be very episodic. And so I think this leads us also to the outcomes and patient reported outcomes piece.
Maybe we can transition into that side, which is, if you’re looking for a greater picture with greater resolution, as well as a deeper understanding of the economics, you also need to understand as cancer patients live longer, we are seeing, I would say, a fortunate unintended consequence, which is what is the long term type of care and impact of quality of life of some of these very powerful interventions, many of which are brand new as it relates to mechanism of action.
I think you have to back up a moment and realize that immunotherapies, CAR-T, some of the viral vectors that are now being used there have not been long term studies in terms of any long term issues that may come from this, because no one’s ever been long term, so I think this is also a very mature way of looking at it.
As someone who is interested in, what are the long-term immunologic or gastrointestinal issues that can follow a successful treatment within immunotherapy, you need a patient to tell you how they’re doing, because we simply don’t know outside of the clinical trial realm, which is very episodic.
So I would say what we’re trying to do is extend the view of the impact of these medicines far outside of the acute care setting or the clinical trial setting in order to have a more full understanding of the risks and benefits.
If you take the first concept, which is we’re measuring all along the way in a common system, we can then do comparisons to understand how these things occur. Some of the benefits tend to be the amount or depth of information, the genetic markers, be it economic, and then the other dimension of it is looking at the total lifecycle or extending the episode of care so that we more fully understand the impact of the medicines or risks.
And we’re not just talking about effectiveness, right—because that’s simply how it translates beyond the trial setting—but also quality of life and long-term adverse outcomes?
DH: That’s right. And again, I think an important part for us is to back up and realize that these are drugs with new mechanisms of action. It really is an incredible time of innovation and pharmaceutical development, and this is all on the shoulders of understanding the biology as elucidated by the genome and all of the research that’s gone on in the 17 years since the genome was published.
We understand the biology relatively well. What we don’t understand is the full medical picture of the intervention and this gets us to that.
The final product program is, obviously, taking patients beyond just matching to clinical trials by improving the enrollment process.
DH: Right. You know, there is a point where waste in health care benefits nobody. There is no entity in this ecosystem that benefits from the waste.
So if we are able to speed drug development with greater precision on which patient goes on which trial, there are operational benefits on the site side, meaning our coordinators simply do less work in order to accomplish their goals, which is access to experimental medicine in the community setting. That’s very important to see at CHI and Dignity.
These sorts of information systems, we use every day in our lives, but very few times have we harnessed that together with the goal that really is aimed towards oncology clinical trial development. Everyone benefits when the right patient is put on the right trial. It decreases the cost of drug development; it decreases the cost of running a site-side research program.
Again, when you eliminate waste from the system, the benefit is primarily to the patients and there are peripheral economic benefits later. Hopefully this could impact the overall cost of drugs, although I will put an asterisk and say that’s speculative.
But theoretically, everyone can agree that information can drive better decisions that make the overall system more streamlined, and we are certainly in need of those things. So when you look at all the dimensions that can help the efficiency and impact of medicine, understanding biology of the patients is a very large piece of this.
So, what is that contribution to it and how do we unpack that so as to make our clinical decisions policy decisions? I would say the first wave in precision medicine was, every drug was unique, meaning each mechanism of action in the drug-gene-indication matrix, each one was a new entity that could solve a problem.
Now we’re comparing across and within drug classes, there are drugs competing against each other, and to understand who goes on what, when is it worthwhile to run a trial, and if we truly believe that we’re moving into an era in which molecular mechanism of tumor is as important as what tissue it came from, then you really need to be able to prove that and you can’t do it with thousands of randomized studies asking one question each. You really have to be able to use it to weave clinical research into the fabric of community cancer care so that you’re asking the questions as you’re looking for the solutions. These platforms allow that.
There is such a strain on resources to stay current, and it is not possible for someone to be able to effectively perform at the quality levels they want with the RVU-like systems and the physician-scientists keeping up with every primary publication. It is it is not possible. The complexity is way too far in this field.
With this new suite of tools slated for development and subsequent integration into Syapse, how robust will the platform be compared to other clinical decision support programs in oncology?
DH: As important as the core technology is, it’s about bringing the ecosystem together. And Syapse has been effective in doing this on a common platform. For example, they support the TAPUR trial and so they’re starting to connect the dots from industry, drug developers, obviously molecular diagnostics, groups like mine that bring to bear a cohesive strategy to hundreds of cancer care providers. And then you’re able to leverage that with payers and other groups in order to give that broader picture and deeper understanding.
I would say there’s a lot of noise going on as this industry matures and to really bring together the right constituents in the ecosystem and have them communicate in an honest way is reflective back to some of the things that [former Vice President] Joe Biden said, and these things happening in a very real way.
You could give all the power points in the world until you bring these people together and we’re able to look at a cohesive single source of truth. Without the data, you’re never going to get anywhere.
How does Syapse help facilitate interactions with payers and bring them to the table? How does it make your work as a provider easier?
DH: That’s a great question. Payers want to know, “Will this intervention be worth it?” And what is the total picture as it relates to the benefit of any given pharmaceutical. I would envision that as it relates to Roche and their portfolio, the uninformed payer is a barrier to patient access.
The agreement to come together to get a better measurement of impact in value will eventually lead towards giving the necessary information that allows for coverage determinations and patient access.
That is, with the host of payers that any major health system would be negotiating with?
DH: That’s right. I mean, these tend to be often first announced by the CMS, and you see patient access basically coming off of analyzed data that can help with coverage determinations. But without the information to guide that, you can’t even approach the process.
So, one of the keys here is, the resolution of healthcare is often proximal to the quality of the EMR systems and clinical informatics. This is in a way improving that resolution so that you can ask better questions and have more sure answers.
Did I miss anything?
DH: No, I really do think that the concept of eliminating waste from the health care ecosystem benefits everybody. And so that’s why this sort of hackneyed concept of bringing everyone to the table—that all sounds great. This is actually doing it.
When we last spoke a-year-and-a-half ago, the Moonshot was at a high point, and everyone was laying out blueprints for how things should be done. The field seems to be in implementation mode now.
DH: I’m actually the keynote speaker at the Precision Medicine track for HIMSS [Healthcare Information and Management Systems Society Annual Conference and Exhibition]. I’m going to be sharing my experience about, a year-and-a-half ago, some people get in a room and I say let’s work on this, right? What happens next?
And I think, when we last spoke, it was all very conceptual. I’ll tell you very little strategically has changed. When I pull up the strategic documents from a year-and-a-half ago, I think we had a pretty good understanding of where this was going to go. The progress with providers is what we are most proud of in a short amount of time.
I would say developments like what happens with Roche and Syapse—that helps. It’s almost as if the thing, the concept that we’re trying to bring forward actually has more meat on it and it’s much more mature, and all the more reason to have an active management strategy on this facet of medicine. Really, really exciting.
And this is moving rapidly in the community setting, no longer just within academic oncology.
DH: That’s right. Some of the Precision Medicine Alliance’s concepts is to be a fast follower and postmodern in a way that I don’t actually need to build or own everything. It’s about access. And if you look at it from an industrial level at the scale that we’re trying to launch, I would rather bring 95 percent of our patients an 80 percent solution than a 100 percent solution to 2 percent of our patients.
This really has to do withs access and these things just to make the overall field more impactful and equitable, because we know what we’re doing better and there’s better reason to strategically invest in it.