“I believe in the concept of a universal cancer vaccine,” said Elias Sayour, a pediatric oncologist at the University of Florida. “I think if this fails in a prospective phase III trial, I still believe we can engineer a vaccine that works prospectively.”
This podcast is available on Spotify, Apple Podcasts, and Youtube.
The cover story of last week’s issue of The Cancer Letter was about the potential of COVID-19 mRNA vaccines to improve response to checkpoint inhibitor therapies in patients with lung cancer and melanoma. The finding was published by Sayour and his colleagues in an October Nature paper.
This week on The Cancer Letter Podcast, Sayour joins The Cancer Letter team to talk about his study and why he is a believer in the promise of mRNA vaccines to help improve cancer treatment.
“mRNA seems the best at doing this,” Sayour said. “That isn’t to say that other vaccines couldn’t harness the antiviral response in a similar manner… All I can tell you is in our preclinical models and in our observations, clinical observations as well, we did look at the Pneumovax [a non mRNA-vaccine] as just an example, a vaccine, and it did not confer the same effects as the COVID-19 mRNA vaccine. Based on that, mRNA to us seems to be very unique. But other vaccine designs that leverage these mechanisms through a non-specific manner could also perhaps achieve the same effects.”
Sayour is hopeful that the COVID vaccine will show clinical benefit in the prospective phase II-III trial that is scheduled to begin enrollment in March, since it would be a boon for patients.
“If it works, I do think that’s revolutionary,” Sayour said. “How commercially available it is, how this can address third-world countries that may have poor access to some of these technologies as a manner of eliciting some type of a universal effect.”
If the COVID vaccine does not help cancer patients in the prospective trial, Sayour said he will continue his work. He sees a future where all cancer patients receive some sort of universal cancer vaccine to reawaken their immune systems to help kill cancer cells.
“It’s my hope that now we could have something that’s instantly available to patients at the time of diagnosis, perhaps right before surgery,” Sayour said. “Everybody gets a universal vaccine to basically awaken that immune response against their cancer. And that could be bookended with immune checkpoint inhibitors, other cancer vaccines, other types of immunotherapies, for maximal effect.”
This episode is sponsored by City of Hope Cancer Center. Learn more at cityofhope.org.
Stories mentioned in this podcast include:
- A planned randomized trial will ask an intriguing question: Do COVID vaccines potentiate checkpoint inhibitors?
- How a Montefiore Einstein screening program is changing the history of lung cancer in the Bronx
- MSK’s AML researcher Bayard “Barney” Clarkson, former president of ASCO and AACR, dies at 99
- Paul Engstrom, Fox Chase pioneer of cancer prevention, dies at 89
- Patient advocate David Mitchell, 75, dies of multiple myeloma
- NIH agrees to review hundreds of denied or shelved grant applications
- House passes three-year extension of ACA subsidies with bipartisan support
This episode was transcribed using transcription services. It has been reviewed by our editorial staff, but the transcript may be imperfect.
The following is a transcript of this week’s In the Headlines, a weekly series on The Cancer Letter Podcast:
Jacquelyn Cobb: This week on The Cancer Letter Podcast…
Elias Sayour: I believe in the concept of a universal cancer vaccine. I think if this fails in a prospective phase III trial, I still believe we can engineer a vaccine that works prospectively. The COVID-19 vaccine is poorly engineered as a cancer vaccine. It’s designed to give you a humoral response, a neutralizing antibody response. If it does fail in prospective studies, I believe we could build a better one. However, if it works, I do think that’s revolutionary, because it’s available for all the reasons you stated at the outset. How commercially available it is, how this can address third-world countries that may have poor access to some of these technologies as a manner of eliciting some type of a universal effect. We’ll be asking many questions about, well, what other cancers does it work and how can we rationally combine? And so, that would be very exciting if this vaccine works, but it has to be validated in prospective studies.
Paul Goldberg: You’re listening to The Cancer Letter Podcast. The Cancer Letter is a weekly independent magazine covering oncology since 1973. I’m your host, Paul Goldberg, editor and publisher of The Cancer Letter.
Jacquelyn Cobb: And I’m your host, Jacquelyn Cobb, associate editor of The Cancer Letter. We’ll be bringing you the latest stories, groundbreaking research, and critical conversations shaping oncology.
Paul Goldberg: So, let’s get going.
Jacquelyn Cobb: Hello, everybody. Packed house today, four people. I don’t know if this is the first time, but lots of people. So, bear with us if there are lots of voices, please. I’ll just introduce quickly: Sara and Paul are both here with me. Sara’s a reporter at The Cancer Letter, and Paul is obviously the editor and publisher. And then also just to introduce before I go into my spiel, we have Dr. Elias Sayour, who will talk about his study and our kind of long relationship with him about… The study came out in October, so we’ll dive into that. I’m getting ahead of myself a little bit.
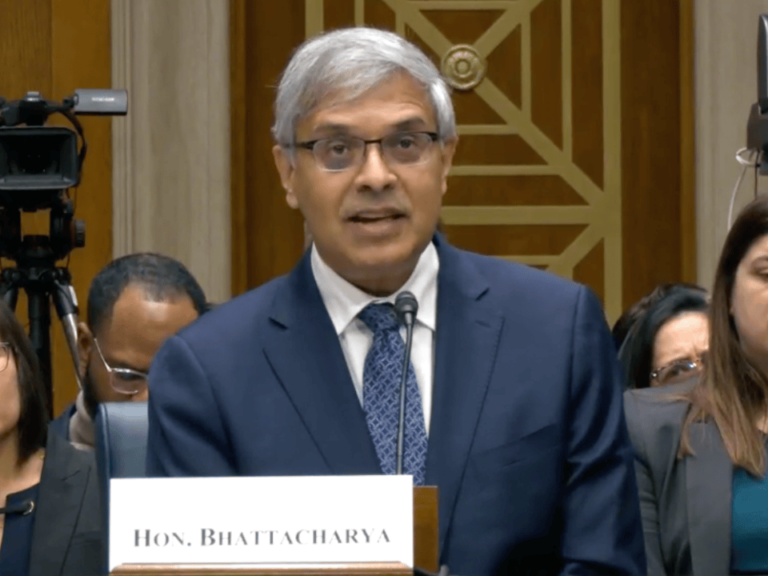
So, last week, our cover story was about Dr. Sayour’s study. It showed that the receipt of a COVID mRNA vaccine within 100 days of initiating checkpoint inhibitor therapy was associated with pretty significantly improved survival outcomes for patients with lung cancer and melanoma.
Jacquelyn Cobb: I really have to restrain myself. I want to talk more about it, but I’ll wait. And just to introduce Dr. Sayour’s titles properly, he is a pediatric oncologist at University of Florida, and he was the senior author on the paper. And the rest of the issue last week was heavily guest editorial driven sort of. We had a guest editorial by Brendon M. Stiles from Montefiore Einstein Comprehensive Cancer Center about his institution’s success at improving lung cancer outcomes, clinical outcomes in the Bronx through coordinated screening efforts and systematic follow-up. So, that was an awesome sort of public health outreach story that was really uplifting.
And then on the other side of things, we had three obituaries last week, but first was written by Paul. And we don’t always write obituaries, but Paul took this one on and I’m so glad he did. It was so, so interesting. And I’ll have him explain that later in the episode. But the other obituaries were for Paul Angstrom, a cancer prevention pioneer and a longtime member of Fox Chase Cancer Center. And David Mitchell, a multiple myeloma patient advocate who was on the board of the Friends of Cancer Research and a pretty common consumer representative of the Oncologic Drugs Advisory Committee.
Cancer policy was packed as always and included stories on NIH agreeing to review hundreds of denied or shelved grant applications. And also we had a story about the House’s passage of a three-year ACA subsidies bill, but we will see how that does in the Senate. So, now with all of that, those words, lots of words out of the way, I’m going to pop it over to Sara to have a conversation with Dr. Sayour about his study and the story that we wrote.
Sara Willa Ernst: Hi, Dr. Sayour. Thank you so much for being with us. Why don’t you just walk us through some of the basics? What are the main findings of the study? And from those findings, what surprised you and what was more in line with what you expected?
Elias Sayour: Yeah, thank you for having me here. It’s an honor and privilege. Yeah, this study was a surprise in many ways. It really was a retrospective study that was really looking at whether we can achieve the effects we were seeing in our preclinical models with mRNA vaccine, now in a real world study with a non-specific mRNA vaccine. We had made this discovery in around 2018 that non-specific mRNA vaccines could awaken the immune system essentially in such a way that could confer sensitivity and response to immune checkpoint inhibitors and otherwise resistant preclinical cancer models. And while this discovery was made prior to the pandemic, the pandemic really allowed kind of this real world scenario now to test whether another form of a non-specific mRNA vaccine. Now the SARS-CoV-2 mRNA vaccines could also sensitize response to immune checkpoint inhibitors in melanoma and non-small cell lung cancer patients, again, looking backwards retrospectively.
And so in collaboration with MD Anderson Cancer Center, we found a near doubling in effect in those patients, patients with melanoma and non-small cell lung cancer within 100 days. We looked at within 100 days of receiving a SARS-CoV-2 mRNA vaccine if they had improved outcomes. And again, at least retrospectively, it appeared that they did.
Sara Willa Ernst: What could something like this mean for access to patients, especially when we’re talking about the context of personalized vaccines, which could cost tens or maybe hundreds of thousands of dollars for some patients?
Elias Sayour: Yeah. This is really something that we think could be deployed at scale universally in a way that is quite cheap. The SARS-CoV-2 mRNA vaccines were so revolutionary because it really allowed us not just to customize a vaccine for the population writ large, but really the ability to even change it. The SARS-CoV-2 mRNA vaccines are updated to stay ahead of the viral evolution. And so, to be able to update these vaccines just by updating the sequence and deploying them, I think, allows us to make cancer vaccines that we can change in a personalized manner. And certainly in a universal manner, the affordability of something like this that you can deploy at scale as now we’ve seen around the world.
It’s my hope that now we could have something that’s instantly available to patients at the time of diagnosis, perhaps right before surgery. Everybody gets a universal vaccine to basically awaken that immune response against their cancer. And now that could be bookended with immune checkpoint inhibitors, other cancer vaccines, other types of immunotherapies for maximal effect.
Sara Willa Ernst: So, this study looks specifically at the mRNA vaccine. I’m wondering, in order for patients to see this benefit with overall survival, how important do you think the mRNA part is? Like could we see this, potentially this type of benefit with other types of vaccines?
Elias Sayour: Yeah, it’s a great question. So, when we made this discovery around 2018, we found that there was a mechanism behind this discovery and the mechanism is largely an antiviral mechanism. A viral response mechanism that leads to type 1 interferon can awaken the immune response. Now, it isn’t as simple as just flooding the immune system with type 1 interferon. Type 1 interferon is this alarm, this 911 call that can lead to other important players, the right cell types, chemokine, other cytokines. And the orchestration of these effects we think awakens the immune response. That seems to us to be most closely aligned with antiviral signals for immune response. So we think mRNA harnesses this antiviral response in a pretty profound manner. However, other vaccines could also activate this antiviral response in a similar manner. It’s not clear to me which other ones could do this. From what I could tell you is mRNA seems the best at doing this.
You’re talking about nucleic acids and a nanoparticle structure, which is essentially what a virus is. So that isn’t to say that other vaccines couldn’t harness the antiviral response in a similar manner that elicits a type 1 interferon response with a cytokine-chemo cascade that is orchestrated in such a way that can awaken and sensitize response. All I can tell you is in our preclinical models and in our observations, clinical observations as well, we did look at the Pneumovax as just an example, a vaccine, and it did not confer the same effects as the COVID-19 mRNA vaccine. Based on that, mRNA to us seems to be very unique. But other vaccine designs that leverage these mechanisms through a non-specific manner could also perhaps achieve the same effects.
Sara Willa Ernst: And I’m just curious, the Pneumovax vaccine, what kind of vaccine is that?
Elias Sayour: The Pneumovax vaccine is the pneumococcal vaccine, it’s the conjugated pneumococcal vaccine that patients get at 65 years and older. We felt this was a good control because most patients at that age will be eligible for that vaccine. And since we were treating an older patient population, wanted to see if that vaccine could also elicit the same effects as the COVID-19 vaccine, and it did not, again, at least retrospectively. And I can’t highlight how important it is to validate these results prospectively. This is so important. I believe in the concept of a universal cancer vaccine, I think if this fails in a prospective phase 3 trial, I still believe we can engineer a vaccine that works prospectively. The COVID-19 vaccine is poorly engineered as a cancer vaccine. It’s designed to give you a humoral response, a neutralizing antibody response. So, if it does fail in prospective studies, I believe we could build a better one.
However, if it works, I do think that’s revolutionary because it’s available for all the reasons you stated at the outset. How commercially available it is, how this can address third world countries that may have poor access to some of these technologies as a manner of eliciting some type of a universal effect. And we’ll be asking many questions about, well, what other cancers does it work and how can we rationally combine it? So that would be very exciting if this vaccine works, but it has to be validated in prospective studies.
Jacquelyn Cobb: Hold on guys. We will be right back after a word from our sponsors.
Life moves fast. It’s fierce, persistent, determined. At City of Hope Cancer Center, they are too. Their groundbreaking research and discoveries have impacted millions of lives globally. They’re moving science forward with the hope, passion, and speed every diagnosis deserves for a cancer-free future. City of Hope, pursuing cancer cures at the speed of life. Learn more at www.cityofhope.org.
Paul Goldberg: We are really now at a point with this study where you have a basic science hypothesis, which has been validated in a retrospective trial, and now you’re going and doing this perspectively. And that we thought that would be an interesting story to put on the cover in part because of the politics of mRNA. Can we talk about that? Could we have you run into that? Have you had any difficulty getting funding? How was the funding situation handled?
Elias Sayour: Yeah, these are very good questions. I’ll try to be thoughtful about how I respond to these. Generally speaking, I think this setting of therapeutic cancer vaccine is very different from the true prophylactic setting, trying to prevent something before it happens. There have been, I think, a lot of concerns raised around prophylaxis, preventing disease, a lot of misinformation around that, by the way, which I find very concerning as a pediatrician. But nonetheless, the prophylactic setting is different than what we’re trying to do here, which is a treatment setting. We’re trying to treat something in cancer after it’s already started. And it is my understanding that despite some of the acrimony around preventative vaccines, again, misinformation as well that I’m not going to get into.
There’s been a lot of support, as I understand it, for therapeutic cancer vaccines. And that support, I think, has extended through all levels of our government. So I don’t have concerns as it pertains to therapeutic cancer vaccines. This around COVID-19 vaccination as a treatment vaccine is a little bit unique because you’re talking about a preventative vaccine now that can be used in the therapeutic setting. So I would think though that based on some of the comments that have been made by our HHS supporting mRNA cancer vaccines, I don’t know why that wouldn’t extend to the COVID-19 vaccine if indeed it is a therapeutic cancer vaccine, which is how we believe it’s working in the context of this last paper.
Paul Goldberg: And you’re talking about mRNA only because that’s what you worked with, because it could, in principle, work out pretty well with peptide vaccine as well.
Elias Sayour: It’s possible. I mean, I… Our study that we… Again, this was based on the MD Anderson data set really showed that mRNA works in a unique manner relative to the other vaccines that we compared it against. Now, we did not do a comprehensive exhaustive review of every vaccine, nor did we have the data to do that. And I do think that nucleic acid vaccines in general, viral vectors that are being used to deliver vaccines, those are some very prime examples of other technologies that may elicit a non-specific immune response, like a sensitized response to checkpoints. I think we should certainly look at those. Peptides, they generally need adjuvants to elicit their effects. And so it’s coming less from the peptide and more from the adjuvant, at least the innate effects. And I’m generalizing, so just bear with me on generalizing here. But those vaccines may not elicit the same effects as these mRNA vaccines.
Now, could you design one to elicit the same effect? I believe absolutely you could. And there may be some that are available, but we haven’t, again, done an exhaustive search retrospectively of whether these vaccines can sensitize response. The ones that we’ve looked into doesn’t seem to be the same effect. MRNA though has significant advantages over… Even if peptides do work, I mean mRNA to be able to make something at scale and engineer it and change it, I think is going to be very advantageous for the future, not just of personalized vaccines, but even universal constructs that we’re creating.
Paul Goldberg: Yeah. I guess, maybe the last question I have is, can we talk about the structure of the prospective trial?
Elias Sayour: Yeah, I’m happy to talk about the context of this trial, which to me is the next step. When we publish this paper, there are groups that have reproduced our results. There are groups that haven’t reproduced our results, which there are flaws to retrospective studies. Retrospective studies are fraught with selection bias. Again, we believe in this concept, we believe in our data. The question though as to whether SARS-CoV-2 mRNA vaccines prospectively will enhance and sensitize response to checkpoints, that remains to be determined. I think this clinical trial needs to be run with all speed to answer this question. It’s in the public centers. And even if it works, I still think we should be working on a better universal vaccine strategy. So whether it works or it doesn’t, there are questions here and you’re getting at some of these questions, which is, well, what is the mechanism for response? How best to do this? How best to engineer it?
My bias is mRNA is going to allow us the capacity to really build these in a way that works better and is in a cost effective manner. But for this trial, we’re restricting this to non-small cell lung cancer patients. We want this to be focused towards that patient population based on the data and the original paper. And we’re really going to be looking at a narrow window, certainly within 100 days of whether patients receiving those vaccines have basically improved response to standard of care therapy, which is either immunotherapy with checkpoint inhibitors or chemo-immunotherapy or for patients with non-small cell lung cancer. This will be, this is not placebo-controlled. We’re trying to make this a pragmatic study real world where we would be looking at patients who are randomized to either getting vaccine or not.
And we believe a single vaccine in a compressed time window from checkpoints could awaken the immune response. And we’ll be running a feasibility trial into a phase 3, so kind of a phase 2, phase 3. We’re trying to… There’s people who may not want to be randomized based on… So there are going to be people who say, “Don’t ever give me a COVID vaccine.” And they’re going to be patients who say, “Well, I’m getting it either way.” There are other vaccines patients can get as prophylaxis to COVID-19, Novavax as an example. And so we don’t know what that dropout rate is going to be for patients who don’t want to be randomized. So, we want a bit of a lead-in into this phase 3 to help us power it, but ultimately this is a pragmatic real-world trial, a randomized trial looking at randomization to receiving that vaccine or not within this time window.
And I should mention, this is a complete partnership with MD Anderson Cancer Center. We have been partners in this and have been very grateful to this partnership, their data sets. So, they have a consortium and we have a consortium here at the University of Florida. We have the OneFlorida Consortium. They have a consortium. So the two of us as lead sites working within these consortiums, we’re hopeful that this will help us enroll patients quickly and answer these questions as quickly as possible.
Paul Goldberg: How many patients do you need?
Elias Sayour: Right now, we’re at about 800 patients to answer this question.
Paul Goldberg: And that you have them or are you thinking of that number?
Elias Sayour: 800 to power this study for a phase III endpoint.
Paul Goldberg: Okay.
Jacquelyn Cobb: Awesome. Well, I would just love… I think as you were talking, I haven’t thought this through, so I might be putting my foot in my mouth a little bit, but it is an interesting question of cancer patients typically are recommended to get the COVID vaccine because of being somewhat immunocompromised generally. So I guess, I’m wondering about the ethics almost of… I mean, obviously, if somebody doesn’t want the COVID vaccine, there’s personal autonomy, but of randomizing with something that we have data that helps people…
Elias Sayour: Yeah, great question. You can’t ethically randomize someone if there’s a therapy that we recommend and is effective. And yes, all cancer… We recommend as oncologists, all patients are vaccinated and are up to date with their vaccines now, but it doesn’t have to be an mRNA-based vaccine. So there are other vaccines for COVID-19 and we would recommend those for those patients. If a patient’s going to enroll on study, we would recommend that they’re vaccinated for COVID-19 and it could either come from the COVID-19 mRNA vaccines if they’re randomized to that arm, or if they’re not, we would recommend that they receive the Novavax, but that would be entirely up to them.
Jacquelyn Cobb: And is that… So, are you looking at sort of the difference between mRNA and the peptide Novavax, or is it just another option?
Elias Sayour: Did that as a sub-analysis, that was mentioned. So, the patients that are randomized to not receiving the mRNA vaccines who opt to receive a Novavax vaccine, would there be differences, right? So, could you kind of do a sub-analysis of the patients who do go on to receive another vaccine versus the mRNA vaccine versus the patients who don’t receive any vaccination at all? Yes. We are planning on looking at that.
Jacquelyn Cobb: That sounds really exciting. Do you have… I know the last that we heard was roughly around March maybe. Do you have a scheduled enrollment day or date?
Elias Sayour: We’re trying to get funding. This is a massive study and will require a significant amount of funding. Again, very grateful to Dr. Griffin, Dr. Lynn, others at MD Anderson Cancer Center who were tremendous partners in this. And that partnership extends the funding, us helping raise money, they’re working on raising money. And we have enough money to start, which has been largely philanthropic, to be honest. We’re working on bigger grants to secure for this, but we believe we can at least start the initial phase of this, which again is phase 2 to 3. And we’re still hopeful that March is reasonable, at least to start at the main institutions, the University of Florida and MD Anderson Cancer Center. We’re still hoping.
Paul Goldberg: What about NCI and the cooperative groups? Are they interested?
Elias Sayour: That’s a really good question. We have not discussed with them. It’s been mentioned though, and we will likely try to reach out to them to see other pathways to perhaps broaden this.
Paul Goldberg: Well, it sounds like you already have. It’s page one of The Cancer Letter.
Elias Sayour: That’s right. Thanks to the collective here. You’ve certainly created traction in ways I wasn’t expecting with cancer centers writ large, NCI. So, thank you.
Paul Goldberg: It’s not a traditional pathway.
Elias Sayour: Yeah, it’s not. But when you’re hearing about The Cancer Letter from other people, other cancer centers. It’s certainly made a lot of headways, so appreciate the shout out. I think I would really just want people to take away from this that we need to run prospective studies. We’re not saying that everybody needs to go out and get their COVID vaccine. I think that’s really important. We believe in the science. We think this is science that warrants new studies, that warrants new universal backbones. We do believe that this concept could really help patients get better responses to immunotherapy and hope that this is a new avenue for more and more research, even if this trial doesn’t work as intended.
We’re hopeful it will, and we think both of those things can now move forward in parallel, having a universal vaccine that’s available while we work on better constructs. But there’s a lot of work left to be done and the excitement around it is something I hope will continue. This is a theme that is unfortunately a little divisive and hoping that the excitement carries through.
Paul Goldberg: Well, thank you very much.
Jacquelyn Cobb: Thanks for being here.
Elias Sayour: Thank you.
Jacquelyn Cobb: Okay. So Paul, now we’re going to switch over to you to talk about your story. We had a full podcast already, but I do think that your reporting really deserves some time to talk about it and hear the story behind the story. I feel like this is key podcast material, so I definitely wanted to hear your experience with that.
Paul Goldberg: Yeah. It’s interesting. I guess, there’s a lot of housekeeping details here that I’m going to divulge. With obituaries, it’s really sometimes great to have them written by people who knew the folks we’re writing about and colleagues. And it’s always, always really interesting. But sometimes I feel like I need to jump in and do a real story because… And we don’t do the kind of ghoullish thing that like the New York Times does when they prepare an obituary for somebody. We don’t do that, but no, there are obituaries written ahead of time, like years sometimes.
Jacquelyn Cobb: Oh, I see what you mean. Yes, yes, yes. Oh my God.
Paul Goldberg: Yeah. So they’re just waiting to push publish. So this last, well, recently, Bayard Clarkson known as Barney Clarkson died and he was 99 years old. I met him, I’m sure. I didn’t know him well. He was not one of those people that I call all the time by any means. I’m pretty sure that Jim Holland introduced us, I think, but I can’t be really sure. And then I’m starting, I’m looking at the obit that we got from Memorial Sloan Kettering and looking at the AACR tribute to him, the ASCO… And I’m thinking, “No, this guy is… Something else is really happening with him that’s really interesting.” And then I started digging and I find his history, which completely just blew me away. And this is late Thursdays, so I discover his oral history that he did for this place called…
Jacquelyn Cobb: The American Field Service.
Paul Goldberg: The American Field Service, which ran ambulances in World War I and II. And he was one of the ambulance drivers for the American Field Service in World War II, shipped out to Italy. Well, first he tried to enlist in the US military, but didn’t get in because they found out that he had inactive tuberculosis. And this is a kid out of high school out of St. Paul’s. And this is also an era when people of privilege, which he was, his family was a banking family. His father was president of the Chase Bank, National Bank, and also American Express. So he wanted to enlist and fight and he did. He didn’t fight, but he ended up shipping out to Italy, getting through Europe, ended up at this camp that they had just found called Bergen-Belsen. And this is near the very end of the war. And it’s just horrific what was going on. 500 people a day were dying from malnutrition.
And his task was every morning, he would put on a canvas suit and big gloves and carry people out of these barracks where the Nazis kept them. And these are people weighing 50 pounds, dying, taking them to a place called the human laundry and where they would be deloused and kind of later put on the floor on these bags, on these mattresses made out of straw, filled with straw. And some would recover and some would not. So he told this story in incredible detail. And he also told about how… And he told that, again, to the American Field Service in this hour long oral history, which I think we cited in the story. And I really hope, in fact, I request that anyone who stumbles across it, click on that and listen to it. It’s just unbelievably cool. And then how he actually kind of put it away for a while.
Didn’t think about it very much or tried not to. Who knows? For 50 years. Except he talked about it. He first went to Yale after the war when he decided to become a doctor, and at Columbia as well. And then he would be at what is now MSK taking care of patients. And he would see a tattoo and he would say, “Where’d you get the tattoo?” “Bergen-Belsen.” “Oh, I was there.” “You were there?” This very Patrician young doctor saying I was there is kind of fascinating. And then 50 years later, he was at a medical meeting in Germany when he ran into Bob Mayer of Harvard and he told Bob Mayer, said, “Oh, I was just with my daughter and I were just at Bergen-Belsen.” He said, “Hmm, I’ll go.”
So he rents a car, drives out, and then it just all kind of pours back and he just all gets back and it hits him hard. So what an amazing character, what an amazing guy. And by the way, he was also president of ASCO in AACR. He was also a very serious researcher. And another irony there is that he was working with what amounts to derivatives of mustard gas, which is to make the first sort of chemotherapies. So really interesting. I ended up kind of getting up around 4:00 in the morning on Friday to go through the hour long Q&A, his oral history and went through it. I think we didn’t… It’s not enough to do justice to someone like that.
Jacquelyn Cobb: But it’s nice because-
Paul Goldberg: Yeah, no, it’s every now and then… It’s interesting because I knew two people who had been through the camps and both had something to do with MSK. The other one was Saul Green, who was a GI who liberated one of the satellite camps in Dachau.
Jacquelyn Cobb: Jesus.
Paul Goldberg: Interesting. Interesting guy. Kind of changed his entire life. Yeah.
Jacquelyn Cobb: Yeah. Yeah. I mean, how could it not?
Paul Goldberg: Yeah. Yeah. It’s an obit I did too. He later became a quackbuster and was kind of a fun character. Anyway, but that’s kind of a neither here nor there issue. But yeah. So here it is. It blew me away. I’m also trying to get in touch with the family. So if anybody knows his daughters… I’m told, I don’t know if it’s true, that he might have a book that he completed that may not have been published. If that’s the case, that’s what The Cancer History Project is for.
Jacquelyn Cobb: Literally.
Paul Goldberg: I’m hoping we could either publish it or bring it back or something.
Jacquelyn Cobb: Yeah. That would be amazing.
Paul Goldberg: No, it’s an amazing story. It really moved me and I probably didn’t do enough of a good job in figuring out what happened to his whole career.
Jacquelyn Cobb: Well, no, that’s what I was going to say though, was that if you didn’t wake up at 4:30 and whatever, we wouldn’t have gotten what we did. And the quotes, I think, from the oral history, which I haven’t listened to yet, but I read in the story, are just incredibly powerful. It would be hard to speak about it in a not powerful way. It’s such an intense experience, but I think the way that he described it was just really incredible too. Thank you, Paul. I will see you next week, and thanks for hopping on and chatting with me about this. I love it.
Paul Goldberg: Yeah. Well, thank you, Jacquelyn, and to everyone else. Thank you for listening.
Jacquelyn Cobb: Thank you for joining us on The Cancer Letter Podcast, where we explore the stories shaping the future of oncology. For more in depth reporting and analysis, visit us at cancerletter.com. With over 200 site license subscriptions, you may already have access through your workplace. If you found this episode valuable, don’t forget to subscribe, rate, and share. Together, we’ll keep the conversation going.
Paul Goldberg: Until next time, stay informed, stay engaged, and thank you for listening.