City of Hope researchers published preclinical research in Nature Communications demonstrating that a CAR-engineered T-cell therapy worked against ovarian cancer in the laboratory and in preclinical models.
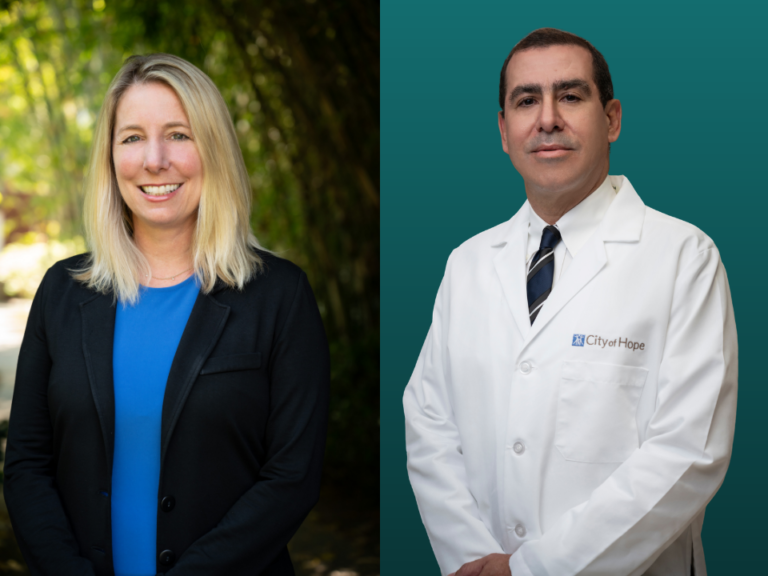
“City of Hope’s research helped develop CAR T-cell therapies for blood cancers, and these patients are now seeing long-term benefits from the therapy, but we can’t stop there,” Saul Priceman, associate professor in the Department of Hematology & Hematopoietic Cell Transplantation and associate director of Translational Sciences & Technologies in the T Cell Therapeutics Research Laboratory at City of Hope, said in a statement. “The next frontier is solid tumors, and City of Hope is taking on that challenge.”
The therapy is currently in a first-in-human phase I trial at City of Hope for patients with advanced epithelial ovarian cancer who have already received platinum-based chemotherapy.
The trial, led by Lorna Rodriguez-Rodriguez, professor in its Division of Gynecologic Oncology in the Department of Surgery at City of Hope, is testing the therapy’s safety, side effects, and activity in patients. The trial is currently enrolling patients for treatment.
The team’s most recent research found that a CAR T-cell therapy targeting TAG72, a target found on the surface of ovarian cancer cells, eradicates cancer cells in mouse models.
“What’s exciting about this is that TAG72 is also found on other cancer cells, including pancreatic, colorectal, breast, and brain tumors, so if the clinical trial in ovarian does well, we can investigate expanding this to other patients,” Priceman said.
Priceman and his team also found that by adding the cytokine Interleukin-12, a protein that sends signals to the immune system, to the CAR T-cell therapy, the treatment worked more effectively against cancer cells in the lab. The co-first authors Eric Hee Jun Lee and John P. Murad, along with the rest of the team, showed that IL-12 also enabled the T cells to fight the cancer, leave the tumor area, enter the bloodstream, and target other cancer cells around the body. IL-12 is not currently part of the current phase I clinical trial.
The preclinical research also found that delivering the CAR T-cell therapy via an injection where the cancer is located, regionally, is also effective in enabling CAR T cells to target cancer elsewhere. This technology allows for both safety and improved anti-tumor activity in several cancer types tested to date.