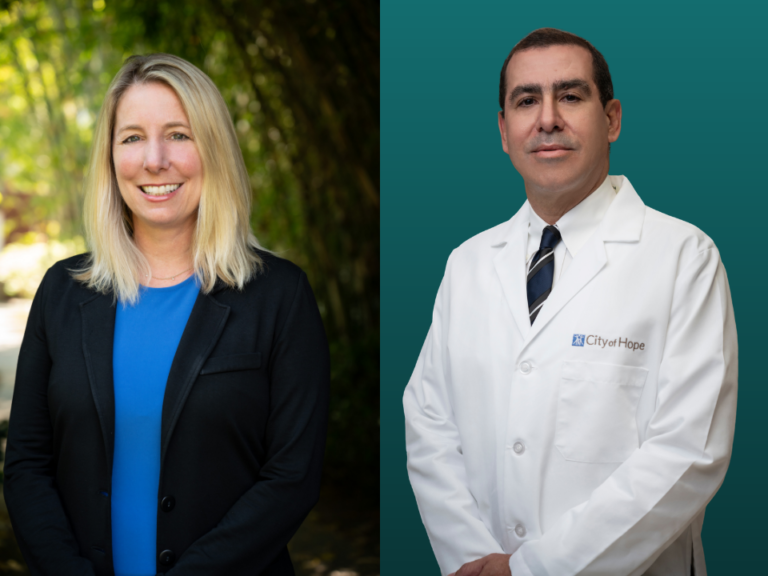
Don’t try to convince Col. Susan Fondy that lymphedema doesn’t merit interest from medical researchers.


After a 20-year career as a military flight surgeon—and exposure to carcinogenic burn pits during her deployments in Iraq and Afghanistan—Fondy was diagnosed with stage 3 breast cancer. While she was still on chemotherapy, she developed lymphedema, an incurable, progressive disease, from the damage her cancer treatment did to her lymphatic system.
As the former chief surgeon of the Army National Guard—the physician in charge of the health and medical readiness of over 300,000 men and women in uniform—Fondy has both an MD and an MPh after her name and doesn’t require a lecture on the principles of public health.
But as someone living with lymphedema, she is disheartened to see lymphedema research profoundly affected by the current assault on biomedical research. “It is incredibly frustrating to me that all the steps that we took are threatened to be taken away,” Fondy said to The Cancer Letter. “I don’t want people who are diagnosed with lymphedema today to have the same experience I had. And to some extent, that’s what’s happening.”
The impact of President Trump’s cuts isn’t anywhere near final, and between thumps of the ax, Fondy and other advocates for lymphedema patients are keeping a tally of grants being canceled, consolidated, and paused as part of Trump’s sweeping effort to “reduce waste” in government spending and realign research priorities.
- In 2025, lymphedema was removed from the list of studied diseases in the Department of Defense’s Peer Reviewed Medical Research Program. While advocates try to get lymphedema back on the list, the funding for the catch-all PRMRP was reduced from $370 million to $150 million.
- The National Heart, Lung, and Blood Institute’s National Commission on Lymphatic Diseases has been inert in 2025, with its scheduled meeting in February slipping by without a word, advocates say.
- Some grants related to lymphatics seem to have been caught up in the mass terminations and freezes of grants even loosely related to the concepts of “DEI” or “gender ideology.”
- The Chronic Disease Education and Awareness Program, established in 2020 with $4 million in funding, has been zeroed out in Trump’s proposed FY26 budget.
- Lymphedema has had success garnering funding through the Advanced Research Projects Agency for Health, or ARPA-H, which is now facing a $50 million reduction in budget.
- Also, the U.S. Department of Veterans Affairs is facing potential staffing cuts that, while small in number, could put additional pressure on the already-strained healthcare system.


The stakes are high for people with lymphedema. The industry doesn’t regard it as a disease likely to produce blockbuster drugs. This means that if the government doesn’t fund the development of lymphedema therapies, they are unlikely to be funded at all.
“In talking to Democrats [and Republicans] on the Hill regarding this, there was great agreement and passion for what we are trying to do [for lymphedema], but then saying, ‘But we are not in power. It is out of our hands,’” William Repicci, president and CEO of the Lymphatic Education & Research Network, said to The Cancer Letter. “And one thing that is made clear to us is that Health and Human Services is going to be made an example of with severe cuts to their funding.”
And while the government is “making an example” of the Department of Health and Human Services, these patients are in need of dedicated research dollars.
“One of the things we hear quite often from people in the medical field is, ‘People don’t die from lymphedema.’ And the reality is, people are dying every day as a result of the impact of having this disease,” Repicci said. Beyond the increased risk of infection and obesity, the mental health repercussions are staggering.
Said Repicci:
There are the many who contemplate, and too often succeed at, suicide as they deal with a lifelong, incurable, and progressive deformity that limits their ability to conduct beloved activities, work, and intimate relationships.
As generous as society can be with issues they understand, it can also be devastatingly cruel when operating from ignorance.
I recall one LE&RN member calling to say, “When my spouse, who has lymphedema, walks down the street, strangers have tapped her on the shoulder to say, ‘You’re disgusting. You need to lose weight.’ So, now, she refuses to leave the house.”
Beyond funding cuts for lymphedema research and awareness, the president’s FY26 budget request calls for a 2,000-person staff cut at the VA—specifically, 6% of the Veterans Benefits Administration workforce. This is while the budget increases overall spending for the VA.
Earlier this year, Veterans Affairs Secretary Doug Collins said in a memo leaked to the press that 15% of the entire VA would be fired—upwards of 80,000 people. Collins has since disputed the media coverage, saying that the internal memo described a “goal” and not a set plan.
The administration’s FY26 budget request seems to signal a move away from the mass firings that were being considered at the VA, but “the budget request numbers do not fully account for VA’s reform plan, which is still being developed,” VA Press Secretary Pete Kasperowicz said in a statement.
The state of the VA is particularly important to Fondy, who retired from the military in December 2024. She received—and continues to receive—her breast cancer and lymphedema care through the VA.
“I have no idea what’s going to happen,” Fondy said. “It would be good to have some answers, but I’m afraid of what those answers are going to be.”
The Trump administration has said that none of the clinical staff at the VA will be cut, but Fondy is concerned specifically about the staff critical to effective lymphedema management.
“Nobody knows what the VA cuts are going to look like,” Fondy said. “We’ve been told that they’re not cutting anyone who’s doing patient care, but I’m not sure what they consider ‘doing patient care.’ The person who works in prosthetics, who gets my lymphedema garments—I’m not sure if they consider her to be doing patient care. There are a lot of people like that who are our critical enablers in the VA system.”
“We have funerals almost every week”
Day and night, Fondy wears a lymphedema compression garment that encloses her entire right arm and all but the fingertips of her right hand. She has to, or the pain starts.
“If I don’t have the pressure on my shoulder, then my shoulder will ache,” Fondy said. “If I don’t have the garment on at all, it takes about half an hour, 45 minutes, and then my forearm will start to ache and throb. That’s why I have to wear the garment all the time. If I don’t, I know about it.”
Fondy’s hand is permanently bent at an angle from years in the compression glove. A former marathoner and an avid exerciser, she is now unable to put her hand flat on the floor to do a pushup.
Many routine activities—including washing dishes, or drinking a cold soda on a warm day—have become more cumbersome, because she has to avoid getting her garments wet.
Fondy prefers to wear long sleeves in public now, because “people think I just have carpal tunnel if they see the glove,” Fondy said. But if her entire compression garment is showing, she gets questions.


“I get strangers on the elevator saying, ‘What’s wrong with your arm?’ or ‘Did you get burned?’”
Although lymphedema and the lymphatic system has been left behind in medical progress, lymphedema is a life-altering and life-threatening disease for an estimated 10 million people in the U.S.
“If you look at other conditions that have far smaller populations that are affected, they get so much more money,” Fondy said. “Even single conditions that have a quarter or an eighth the number of people who are affected by lymphedema get vast amounts more money.”
Since the lymphatic system doesn’t fall under the purview of any single medical discipline, lymphedema is widely considered an unfortunate consequence of life-saving cancer treatment.
“There’s no particular doctor field that owns it, and so, there’s no one specifically who is responsible for doing research on it,” Fondy said. “And so, we got farther and farther behind.”
The lymphatic system is a central piece of the immune system. As the circulatory highway that carries lymph and white blood cells throughout the body, it collects the detritus of the body—cellular debris, bacteria, toxins—and deposits them in lymph nodes for eventual elimination through the kidneys, liver, or lungs.
However limited, research in lymphedema has yielded important results. One example is the standard-of-care axillary lymph node dissection in breast cancer. In the past, a surgeon by default removed a large number of lymph nodes from a patient’s armpit. Now, this has been replaced with sentinel node biopsy, which calls for the removal of only the first few lymph nodes into which a tumor drains.
But while sentinel node biopsy may be standard practice, advocates say that some surgical oncologists are woefully uneducated about the risk factors for lymphedema.
Fondy, who had gone to medical school and completed two separate residencies—one in pediatrics and one in aerospace medicine—was more equipped than most to advocate for herself during cancer treatment.
Still, her oncologists dismissed her concerns, and she was not given any information about how to reduce the risk of lymphedema.
Said Fondy:
I had already read about lymphedema. I didn’t know a ton about it. I just knew that it was a possibility. And so, my surgical oncologist talked to me about my surgical options. We talked about mastectomy versus lumpectomy and sentinel nodes versus axillary node dissection. And because I had visible metastasis to nodes, that I would probably wind up needing an axillary dissection.
He put his hand on the doorknob facing away from me and turned back and said, “Do you have any questions?”
And I said, “Yes. What about lymphedema?”
His response was, “What about it?”
And so, of course, I didn’t even know how to respond to that. And I said, “Well, I don’t want to get it.”
And his response was, “You won’t. You are small.” Meaning, not obese.
As it turns out, obesity is literally the only risk factor that I did not have. I was young. I was going to be getting an axillary node dissection, I was going to be getting chemotherapy, including taxanes, and I was going to be getting radiation. All of those are risk factors.
He didn’t talk with me about surgical options that they can do early on that can help reduce the risk of lymphedema issues.
And the only thing that they did was they did map which lymph nodes drained my arm. But then they wound up taking out whatever they needed to take out anyway, and not really avoiding those lymph nodes.
He could have said, “Hey, you are at a very high risk for lymphedema. You might want to go here, here, or here where they can do this surgery that will give you the best chance of avoiding lymphedema.” And I would have done that.
But he didn’t know, and he didn’t say.
Fondy’s experience was, unfortunately, commonplace. The options to reduce the risk for lymphedema are not common knowledge for cancer patients, and not often brought up by surgical oncologists.
“There are surgeries like lymph node transfer that can be done moving lymph nodes into the area where the lymph nodes have been removed to continue lymph flow,” Repicci said. “There’s also lymphatic venous anastomosis, also called LVA. Whereas usually, the lymphatic and venous vessels would just be cut and tied-off during breast cancer and other surgeries,instead they are connected.


“It only takes about 15 minutes more to do that. And it allows the lymph fluid to continue its natural journey to the heart. The result has been that this procedure significantly reduces the incidence of lymphedema as a result of breast cancer.
“The reality is, very few patients will ever even hear these were potentially options.”
Lymphedema occurs in an estimated 20-30% of patients with breast cancer. Between 7% to 15% of patients treated for ovarian, endometrial, colorectal, and prostate cancer, as well as patients with melanoma and sarcoma, will also develop lymphedema. Patients with head-and-neck cancers are particularly susceptible to cancer-related lymphedema, with over 70% reporting lymphedema.
It is incredibly frustrating to me that all the steps that we took are threatened to be taken away. I don’t want people who are diagnosed with lymphedema today to have the same experience I had.
Col. Susan Fondy
Lymphedema is a relatively manageable disease for many. But complications can be deadly.
Obesity related to the impact of lymphedema brings its own health challenges and compromises longevity, Repicci said. And often, “heart disease is actually lymphedema in the heart valves.”
Another danger is cellulitis.
“We have funerals almost every week of people who, as a result of the lymphedema, had developed bacterial infections like cellulitis.” Repicci said. “The toxins just accumulate in that part of the body, and infection sets in. Cellulitis is the infection.”
Like any bacterial infection, cellulitis requires antibiotics. But people with lymphedema often don’t realize that the infection is setting in.
“Very often, people don’t even know they have it. It’s subtle. The skin turns pink, etc.,” Repicci said. Also, the skin is often hidden by a lymphedema garment. “If it goes too far and the antibiotics don’t work, people die of sepsis.”
Hard-won successes, slashed
When Fondy was diagnosed with lymphedema, one of her first questions was, “What about flying?”
Her lymphedema therapist put it simply: “You can’t fly.”
“That’s not an option, because that’s what I do,” Fondy replied.
For Fondy, some of the best and most fulfilling times of her life were in the back of a Black Hawk helicopter. Over the course of her decades-long career in the military—including four deployments, flying crafts to the sides of mountains, and teaching Afghan doctors—flying was a necessary piece of the work.
Through this work, Fondy fulfilled a sense of duty she felt called to since 9/11.
“Especially as a deployed physician, there’s a worthiness to the work. You’re taking care of people at their worst moment,” Fondy said. “And you’re able to pull people out of it and send them home to their families.”
This work was her life, and this work required flying.
I’m like, ‘Well, the heck with it. If there’s no actual answer, then I’ll just have to use myself as a test case and find out if my lymphedema gets worse after I fly. And if it does, then I won’t fly.’
Col. Susan Fondy
Even as the chief surgeon of the National Guard, where flying isn’t technically part of the job, she was required to fly every month to maintain her flight status.
“You always have to train for what you’re going to do downrange,” Fondy said. “So, do we fly here [in the U.S., as training]? Absolutely! We have to. If we don’t fly here, then we won’t be able to fly down there. So, I flew every month.”
Cabin pressure changes can exacerbate existing lymphedema, but Fondy’s lymphedema therapist’s recommendation against flying was based on civilian use of commercial airline flights. Fondy’s flights were entirely different.
“I’m thinking about all the different altitudes,” Fondy said. “If you fly commercial jets, you’re pressurizing a cabin between 5,000 and 8,000 feet. I’m flying in helicopters, and we are flying at 500 feet, 1,000 feet, 1,500 feet.”
Fondy’s lymphedema therapist was not particularly helpful, she said. Lymphedema therapists are typically occupational or physical therapists who have taken a nine-day class in lymphedema, according to Fondy.
“It’s not like they go through a two-year program to become a lymphedema therapist,” Fondy said. “Unfortunately, I had several lymph therapists who were along those lines.”
So, Fondy searched PubMed, finding, to her surprise, that research in lymphedema was shockingly paltry.
“I went to PubMed, and I started looking for research on aviation and lymphedema,” Fondy said. “And I found, at that point, a total of four articles. One of them was a case study, one of them was people who were at risk for lymphedema, but didn’t have it. They were all over the map.”
With a dearth of available research, Fondy decided to be her own case study.
“I’m like, ‘Well, the heck with it. If there’s no actual answer, then I’ll just have to use myself as a test case and find out if my lymphedema gets worse after I fly. And if it does, then I won’t fly,’” Fondy said. “So, I started measuring my arm before and after I flew, and seeing how it felt.”
Fondy was able to continue flying, and only ended up missing one month of active flight status over the course of her career—and it was because of chemo treatment, not lymphedema.
“I said, ‘Nobody else is helping me. I guess I need to help myself,’” Fondy said.
Fondy’s experience is a stark example of how lymphedema is in desperate need of increased awareness, education, and research. And the hard-won yet meager successes of lymphedema advocates are now being forgotten, reduced, or zeroed out.
These include:
Peer Reviewed Medical Research Program
Lymphatic diseases and lymphedema had, for the first time in 2023, made its way onto the list of diseases included in the Peer Reviewed Medical Research Program. Through this mechanism, $12 million of research funding came to the field of lymphatic diseases and lymphedema between 2023 and 2024.
In 2025, that budget for the Peer Reviewed Medical Research Program was cut from $370 million to $150 million, and lymphatic disease and lymphedema were both left off of the list.
“So, we are now struggling and lobbying to get those back on the list for next year, with the budgets that have been proposed at this point, there is a proposal to increase that from the $150 million this year,” Lymphatic Education & Research Network’s Repicci said. “The problem, of course, is that they removed many diseases from the Congressionally Directed Medical Research Program, and now they’ve thrown them all into the Peer Reviewed Medical Research Program. So, you have twice as many diseases fighting for half as much money, and now we’re struggling even to get back on the list.”
The National Commission on Lymphatic Diseases
The National Commission on Lymphatic Diseases, established by the National Heart, Lung, and Blood Institute in 2023, “focused on lymphatic diseases so that all of the small lymphatic portfolios spread all over the institutes and centers would now be coordinated in one place with a bigger budget and with the staff to oversee it so that we really could focus on our successes going forward,” Repicci said.
Now, in the second year of the commission, there has been no activity, despite a meeting scheduled for February. Regardless, the commission is “determined to attempt to finish the report on their own, with no idea, at this point, whether NIH will accept it, promote it, print it, etc.,” Repicci said.
Worse, lobbying to support the recommendations of the commission will be a near-impossible task.
“Even once we get this report, lobbying for funding for any of the things that are recommended within this is going to be a struggle, given that, whether it Republicans or Democrats in Congress, the response when you mention Health and Human Services is unfortunately they are going to be made an example of and that there’s nothing that we can do,” Repicci said. “So, we don’t immediately see a turnaround there.”
The Chronic Disease Education and Awareness Program
The Chronic Disease Education and Awareness Program wasestablished in 2020 with $4 million in funding.
The Lymphatic Education & Research Network, the advocacy organization Repicci heads, was one of the original recipients of a grant from the Chronic Disease Education and Awareness Program. With that grant, LE&RN launched an educational website for cancer patients to learn about cancer-related lymphedema.
One of the things we hear quite often from people in the medical field is, ‘People don’t die from lymphedema.’ And the reality is, people are dying every day as a result of the impact of having this disease.
William Repicci
“That has resulted in over 500 people a day visiting the website on cancer-related lymphedema,” Repicci said. “To learn everything you need to know before you have cancer surgery, what to do afterwards, how to treat it, how to talk to your surgeon about it, how to talk to your friends and family about this as well, to nurture you through the process.”
Repicci has been told that although his grant was slotted to be funded again, there may be no money to give out.
“If there was money over the next 24 months, the program could continue and would be funded,” Repicci said. “Right now, I’m looking at the president’s budget for FY26, and the Chronic Disease Education and Awareness Program is completely zeroed out. So, that’s where we stand with that program at this point as we attempt to keep it alive.”
In a disease setting where awareness and early intervention is a key barrier to improved outcomes, cutting an inexpensive education and awareness program is ultimately costing taxpayers money, Repicci said.
“The reality is, if even a few of those people avoid lymphedema as a result of this campaign, you’ve more than paid for the entire annual cost of the campaign itself,” Repicci said.
Terminated and frozen grants
Some lymphatics research grants have been terminated or frozen due to entanglements with “DEI” or “gender ideology.” One such grant was reportedly canceled because it was under an RFA that promoted diversity in the workforce through a summer program for local underrepresented high school students.
The grant has now been reportedly reinstated following the decision by U.S. District Judge William Young for the District of Massachusetts that the cancellations were illegal, but no money has made its way to the researchers at the time of this writing. Plus, lymphatics researchers are reporting that their R01s for the current budget year have expired, while the installment for the next budget year has not been provided.
This delay has “the same effect as termination,” since the funds are not available to support personnel and research, a lymphatics researcher said to The Cancer Letter under the condition of not being identified by name out of concerns for repercussions.
ARPA-H
Two lymphatics-related programs have been created through the Advanced Research Projects Agency for Health, or ARPA-H. Also, the Women’s Health Initiative specifically includes lymphatic diseases as one of the research areas eligible for funding.
LIGHT, or Lymphatic Imaging, Genomics, and Phenotyping Technologies, was launched in 2024 and aims to find comprehensive diagnostic solutions for lymphatic disease. Also in 2024, ARPA-H launched the GLIDE, or Groundbreaking Lymphatic Interventions and Drug Exploration, a program tasked with developing new physical and pharmacological therapies targeting abnormal lymphatic structure and function.
Now, ARPA-H is facing a $50 million reduction from FY25 levels. In the president’s FY26 budget request, $100 million is slated for ARPA-H, compared to $150 million in FY25.
“If the overall funding for ARPA-H is reduced, it will have a profound impact on the trajectory of innovative research aimed at improving public health over the next three to five years,” Repicci said. “This includes setbacks to the discovery of treatments and cures of lymphatic disease, which are only now receiving the attention they deserve.”