This story is part of The Cancer Letter’s ongoing coverage of COVID-19’s impact on oncology. A full list of our coverage, as well as the latest meeting cancellations, is available here.
The COVID-19 pandemic will likely cause at least 10,000 excess deaths from breast cancer and colorectal cancer over the next 10 years in the United States.
Scenarios run by NCI and affiliated modeling groups predict that delays in screening for and diagnosis of breast and colorectal cancers will lead to a 1% increase in deaths through 2030. This translates into 10,000 additional deaths, on top of the expected one million deaths resulting from these two cancers.
“For both these cancer types, we believe the pandemic will influence cancer deaths for at least a decade,” NCI Director Ned Sharpless said in a virtual joint meeting of the Board of Scientific Advisors and the National Cancer Advisory Board June 15. “I find this worrisome as cancer mortality is common. Even a 1% increase every decade is a lot of cancer suffering.
“And this analysis, frankly, is pretty conservative. We do not consider cancers other than those of breast and colon, but there is every reason to believe the pandemic will affect other types of cancer, too. We did not account for the additional non-lethal morbidity from upstaging, but this could also be significant and burdensome.”
An editorial by Sharpless on this subject appears in the journal Science.
The early analyses, conducted by the institute’s Cancer Intervention and Surveillance Modeling Network, focused on breast and colorectal cancers, because these are common, with relatively high screening rates.
CISNET modelers created four scenarios to assess long-term increases in cancer mortality rates for these two diseases:
1. The pandemic has no effect on cancer mortality
2. Delayed screening—with 75% reduction in mammography and, colorectal screening and adenoma surveillance for six months
3. Delayed diagnosis—with one-third of people delaying follow-up after a positive screening or diagnostic mammogram, positive FIT or clinical symptoms for six months during a six-month period
4. Combination of scenarios two and three
Treatment scenarios after diagnosis were not included in the model. These would be: delays in treatment, cancellation of treatment, or modified treatment.
“What we did is show the impact of the number of excess deaths per year for 10 years for each year starting in 2020 for scenario four versus scenario one,” Eric “Rocky” Feuer, chief of the NCI’s Statistical Research and Applications Branch in the Surveillance Research Program, said to The Cancer Letter.
Feuer is the overall project scientist for CISNET, a collaborative group of investigators who use simulation modeling to guide public health research and priorities.
“The results for breast cancer were somewhat larger than for colorectal,” Feuer said. “And that’s because breast cancer has a longer preclinical natural history relative to colorectal cancer.”
Modelers in oncology are creating a global modeling consortium, COVID-19 and Cancer Taskforce, to “support decision-making in cancer control both during and after the crisis.” The consortium is supported by the Union for International Cancer Control, The International Agency for Research on Cancer, The International Cancer Screening Network, the Canadian Partnership Against Cancer, and Cancer Council NSW, Australia.
A spike in cancer mortality rates threatens to reverse or slow down—at least in the medium term—the steady trend of reduction of cancer deaths. On Jan. 8, the American Cancer Society published its annual estimates of new cancer cases and deaths, declaring that the latest data—from 2016 to 2017—show the “largest ever single-year drop in overall cancer mortality of 2.2%.” Experts say that innovation in lung cancer treatment and the success of smoking cessation programs are driving the sharp decrease (The Cancer Letter, Feb. 7, 2020).
The pandemic is expected to have broader impact, including increases in mortality rates for other cancer types. Also, variations in severity of COVID-19 in different regions in the U.S. will influence mortality metrics.
“There’s some other cancers that might have delays in screening—for example cervical,prostate, and lungcancer, although lung cancer screening rates are still quite low and prostate cancer screening should only be conducted on those who determine that the benefits outweigh the harms,” Feuer said. “So, those are the major screening cancers, but impacts of delays in treatment, canceling treatment or alternative treatments—could impact a larger range of cancer sites.
“This model assumes a moderate disruption which resolves after six months, and doesn’t consider non-lethal morbidities associated with the delay. One thing I think probably is occurring is regional variation in these impacts,” Feuer said. “If you’re living in New York City where things were ground zero for some of the worst impact early on, probably delays were larger than other areas of the country. But now, as we’re seeing upticks in other areas of the country, there may be in impact in these areas as well”
How can health care providers mitigate some of these harms? For example, for people who delayed screening and diagnosis, are providers able to perform triage, so that those at highest risk are prioritized?
“From a strictly cancer control point of view, let’s get those people who delayed screening, or followup to a positive test, or treatment back on schedule as soon as possible,” Feuer said. “But it’s not a simple calculus, because in every situation, we have to weigh the harms and benefits. As we come out of the pandemic, it tips more and more to, ‘Let’s get back to business with respect to cancer control.’
“Telemedicine doesn’t completely substitute for seeing patients in person, but at least people could get the advice they need, and then are triaged through their health care providers to indicate if they really should prioritize coming in. That helps the individual and the health care provider weigh the harms and benefits, and try to strategize about what’s best for any individual.”
If the pandemic continues to disrupt routine care, cancer-related mortality rates would rise beyond the predictions in this model.
“I think this analysis begins to help us understand the costs with regard to cancer outcomes of the pandemic,” Sharpless said. “Let’s all agree we will do everything in our power to minimize these adverse effects, to protect our patients from cancer suffering.”
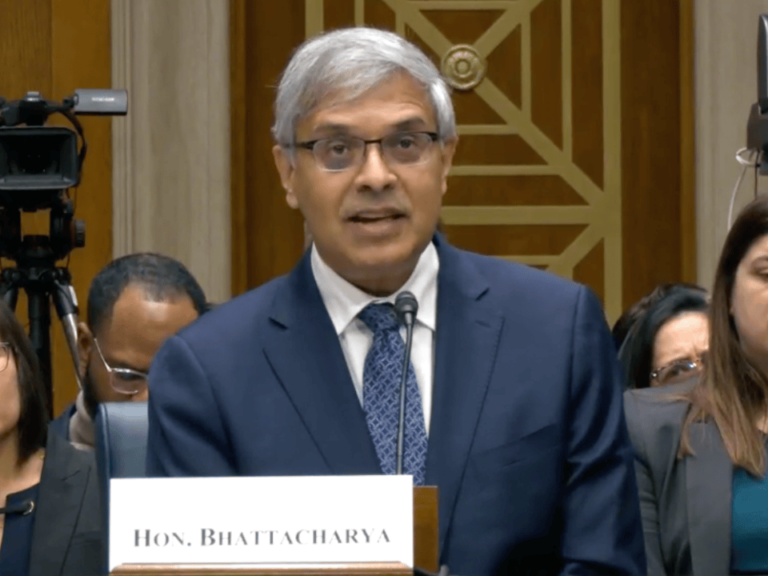
Sharpless’s remarks at the June 15 NCAB-BSA virtual meeting follow:
We are delighted to welcome four new full members to the NCAB today. Dr. Anna Barker, former deputy director of NCI, now at USC. Dr. Howard Fingert, a medical oncologist with significant translational expertise who’s had a long experience advising the NCI and FDA. Dr. Andrea Hayes-Jordan, surgeon-in-chief at the University of North Carolina Children’s Hospital, and Dr. Susan Vadaparampil, vice chair of Health Outcomes and Behavior, the department at the Moffitt Cancer Center. Thank you.
It seems that, lately, each time that we meet, our circumstances have changed in ways that we did not foresee. In early April, we held an extra joint board meeting to focus on the pandemic and NCI’s response. At that point, NCI and many of your institutions had just moved to the mostly telework environment for COVID-related care and research, and we were just three to four weeks into that new way of working at that time. Convening a meeting virtually entirely was still new and the cancer research community was frankly reeling, making urgent decisions with limited evidence on how to proceed forward.
Many of you remember that Dafna [Bar-Sagi] gave us a glimpse into the pandemic’s epicenter at NYU. I reflected at that time on a quote from Hamlet that I like. “When sorrows come, they come not as single spies, but as battalions.” And sadly, that sentiment is still with us today. On May 12, the BSA gathered for a regular meeting, a marathon virtual meeting that reviewed 13 concepts. I know I for one found it reassuring to focus on our bread-and-butter cancer research, identifying and incentivizing this insanely great cancer research that is the business of the NCI.
And now today, just four weeks later, it seems everything once again has been scrambled and changed. The news is now filled with images that are shocking and unforgettable, but also that defy easy explanation. No longer now of crowded ERs and ICUs and ambulances, but instead of police brutality, marches and protests. While we each wrestle with the stark realities of racial injustice that recent events have laid bare, we also have to confront these issues at institutions as a profession, as people who’ve devoted our careers to alleviating suffering.
I’m grateful to the many leaders within our cancer research community who were speaking out on these topics. Something in particular I really admired were two pieces in the recent June 5 issue of The Cancer Letter from Rob Winn, a cancer center director at VCU, and our own Otis Brawley, who’s with us today. For those of you who have not read these pieces, I highly recommend them. And Otis, thank you for your comments on this topic and your lifetime of leadership on these issues.
While we each wrestle with the stark realities of racial injustice that recent events have laid bare, we also have to confront these issues at institutions as a profession, as people who’ve devoted our careers to alleviating suffering.
I anticipate that in future board meetings, we will formally seek the counsel of the NCAB and the BSA on how NCI can enhance our current programs to address cancer disparities and workforce diversity. We also have some new things in the works in this vein that we will want to discuss soon when they’re ready for talking about. In the meantime, as always, we are here to listen.
As a little bit of usual business, I thought I would show a traditional slide that I always show at this meeting, where we are in the budgeting process. Obviously this year’s appropriation process is quite strange and different from prior years. Congress, in addition to working on the 2021 budget, is also hard at work still on a fifth supplement to the 2020 budget. There’s a lot in play on this topic. It’s complicated, and I will leave this to M.K. Holohan to talk about later on this morning. It’s very interesting. A lot going on.
Our primary concern is, of course, the health and safety of people with cancer, healthcare providers and NCI grantees and staff, and we are fortunate and proud to be able to continue to contribute our expertise and infrastructure to the critical research on COVID-19.
We discussed a lot of this at prior meetings so I won’t go into too much detail today, and Doug will be talking about serology a bit more. I will highlight the bottom here on the clinical trials of immunomodulatory agents. That’s a new trial that is opened for tocilizumab and compassionate use, as well as based on a recent paper from Lou Staudt and Wyndham Wilson on acalabrutinib as a potential therapy for severe COVID-19. And even though we’ve had recent presentations on many of these items, I will update you on a few areas of progress very briefly.
Serology and related technologies
So, as many of you are aware, Congress has provided the National Cancer Institute with a large supplemental appropriation for research of COVID-19 serology and related technologies. The history of this is that, in early March, during the early days of the pandemic response, we pivoted our top-notch serology lab at Frederick National Lab, which does regulatory-grade work for HPV, and we’ve moved that lab to work on coronavirus.
We collected a lot of samples of reagents and working with CDC and NIAID, we quickly developed a high quality ELISA assay. In particular, I personally sent about 30 emails to various cancer center leaders and other academics requesting their help, and their response to that was wonderful, with many institutions really helping the NCI with expertise in samples.
While developing reagents, we were approached by the device center at FDA who asked for our help with performance testing.This led to a really exciting and gratifying inter-agency collaboration to test the usability of these devices in real world settings. Serology work at Frederick National Lab and other parts of the NCI continues today at a furious pace with collaborators at FDA, CDC, BARDA, and NIAID.
I should also mention, regarding serology, at the May meeting Dinah Singer shared with the BSA plans for Serological Sciences Network, which we’re now calling SeroNet. It was said then, but bears repeating, really, hats off to Dinah and her team, who mobilized NCI staff incredibly quickly to craft this program. We recently published two new funding announcements (RFA-CA-20-038, RFA-CA-20-039) that will create SeroNet. To meet the urgent need associated with the pandemic, these open RFAs were developed in record time at close on July 22.
We recognize that expertise in these areas is well beyond the researchers usually at NCI’s pool, so we’re reaching out through a number of organizations and channels that are not our traditional stakeholders. I also explained at the meeting how this NCI-NIAID-administered network is not solely cancer-focused, although we fully hope and expect many of the basic science studies to be supported by this network. For example, examine the links between cellular and humoral immunity or studies about antibody structure and function. So, we hope and expect that these sorts of studies will be highly valuable to cancer research as well.
Jim Doroshow shared plans for this study with all of you in April. This is our clinical trial studying COVID-19 natural history in cancer patients, and things on this front have progressed marvelously. You recall this is not a registry, but a trial with informed consent that allows longitudinal collection of samples and data from patients, including imaging results. There will be a robust analysis of serum biomarkers in order to identify predictors of outcome in these patients, as well as analysis of germline genetics. This trial, we’re now calling NCCAPS, launched on May 21 and already has nearly 450 sites activated with plans to enroll 10,000 patients.
Modeling an increase in cancer mortality
At the BSA meeting in May, I spoke briefly about the impact of the pandemic on cancer outcomes, I think something that many of us are becoming more concerned about. We’ve seen decades of great progress with regard to national cancer mortality statistics, and no one wants to see that progress undermined. This slide shows what we should be worried about, the ways in which the global pandemic could disrupt cancer progress.


There’s the issue of delayed diagnosis, because patients are less likely to see doctors for a new symptom or for routine screening during the pandemic. There’s the issue of deferred care, because hospitals and clinics have stopped certain “elective procedures.” Elective, like resection of tumors and elective chemotherapy. And they’ve stopped these elective procedures to preserve hospital capacity during the pandemic. And then, there’s the issue of reduced and nonstandard care during the pandemic.
For example, some centers have been using neoadjuvant therapy to delay surgery for some diagnosed cancers, which is not a standard practice necessarily in those diseases. It’s unclear how these nonstandard regimens will affect outcome. To be clear, we think these hospital closures and pauses were appropriate at the time, but we are also now very much interested in understanding how we get our patients back in the clinic and get care resumed for their benefit.
To get an idea of an estimate of what we think the impact of these changes will be, I asked Rocky Feuer at NCI CISNET, as well as our extramural fundees in this area to help figure this out. I think most of you are familiar with the CISNET network, which does state-of-the-art and cutting edge cancer modeling. I asked them to try and understand the effects of delayed and deferred care on cancer outcomes.
We chose to do this for breast and colon cancer, since these are common cancers with relatively high screening rates. And CISNET investigators had developed sophisticated and validated simulation models that had provided a link between complex evidence and actionable public health strategies for those diseases. We made reasonable assumptions about the effects of COVID-19 on cancer screening and treatment, and modeled the effects on mortality for these two cancers over the next decade.


This analysis, as shown here with the excess mortality plotted by year, it suggests that we will see roughly 10,000 excess breast and colorectal cancer deaths over the next 10 years, which represents a roughly 1% excess in deaths from these two tumor types over that period. For both these cancer types, we believe the pandemic will influence cancer deaths for at least a decade.
I find this worrisome as cancer mortality is common. Even a 1% increase every decade is a lot of cancer suffering. And this analysis, frankly, is pretty conservative. We do not consider cancers other than those of breast and colon, but there is every reason to believe the pandemic will affect other types of cancer, too. We did not account for the additional non-lethal morbidity from upstaging, but this could also be significant and burdensome.
Perhaps most crucially, this analysis assumes only a moderate disruption in screening and care that completely resolves after six months. Obviously, if the pandemic disrupts routine cancer care to a greater degree or for a longer period, the effect on current cancer mortality could be even worse. I think this analysis begins to help us understand the costs with regard to cancer outcomes of the pandemic. Let’s all agree we will do everything in our power to minimize these adverse effects, to protect our patients from cancer suffering.
Notable research
I’d like to briefly show some science from the intramural program. This is a really handsome paper from Tim Greten and colleagues from CCR published last week in Cell. NCI investigators studied biomarkers for liver cancer. This is the largest study to date analyzing serological samples using a high-throughput viral technology in patients with the hepatocellular carcinoma.
Parenthetically, before, I mentioned that NCI has some great serology and biology researchers, as evidenced here. This study shows that viral exposure signatures hold promise for being developed as cancer biomarkers for the early onset of hepatocellular carcinoma. After initial training analysis, the researchers tested their signature on blood samples from 173 people with chronic liver disease who were part of a 20-year study. During that time, 44 of the participants developed hepatoma.
Using blood samples taken when the cancer was diagnosed, the signature correctly identified those who developed HCC with an area under the curve of 0.98. And importantly, the signature also worked when the researchers used blood samples taken at the beginning of the study, up to 10 years before diagnosis, with an AUC of 0.91. These are very promising developments for a cancer where there’s not been a lot of good news and it is of growing importance, both in the United States and internationally.
Here’s another effort of something we were just getting started with that we’ve been working on a long time and to address another very difficult GI malignancy, pancreatic cancer, where there has not been sufficient progress. As many of you know, new-onset diabetics over the age of 50 are at much higher risk of being diagnosed with pancreatic cancer within three years of their diabetes diagnosis. NCI, in partnership with PanCAN as well as NIDDK, has developed a new-onset diabetes study to examine this high-risk population. This will prospectively collect a cohort to follow individuals for the development of pancreatic adenocarcinoma.
The study will establish a biobank of clinically annotated biospecimens. It will facilitate validation of emerging tests for identifying NOD subjects at high risk for having pancreatic cancer using the clinically annotated biospecimen reference set. And it will provide a platform for the future development of an early detection protocol for sporadic pancreatic cancer in new-onset diabetes subjects that incorporates novel imaging as well as other clinical parameters.
Leadership updates
As many of you are aware, we will soon welcome Dr. Phil Castle, I’m told, in early July, as director of the Division of Cancer Prevention. We are extremely grateful to Debbie Winn for her superb work holding down that job in the acting capacity for the past, more than a year.
I am also pleased to announce that Emily Tonorezos will also be joining the NCI as director of the Office of Cancer Survivorship. Dr. Tonorezos is currently at Memorial Sloan Kettering and has specialized in long-term follow up of adult cancer survivors. She’s been selected for the appointment, pending clearance. And I would like to thank our old friend Deb Mayer of UNC, who has been instrumental in supporting the Office of Cancer Survivorship since the retirement of Julia Rowland.
Final word, I’d like to remind you of our Bottom Line blog. We’ve continued to post articles of particular interest to the NCI about concepts, about cancer research in COVID-19 era, about cancer training during the pandemic. I think the response to these posts has been really great, and I hope you found it useful and you’ll continue to spread the word and point others to this as well, where it contains a lot of information for our grantees and other interested stakeholders.