Sometimes in oncology, you get “beat-the-reaper” stories.
- There is the classic story of John Mark Cleland, the first man whose metastatic testicular cancer was cured with combination chemotherapy containing cisplatin. He would live another 47 years.
- And there is a story of Beth Carner, diagnosed with stage 4 colon cancer at age 25 in 2014 and, as a last-ditch effort, treated with a drug now known as Keytruda (pembrolizumab), which targeted her specific genetic mutation—MSI (microsatellite unstable)-H.
- And there is Judy Orem, who, after running out of treatment options for chronic myeloid leukemia in 1998, enrolled in a phase I clinical trial of STI-571, a drug now known as Gleevec.
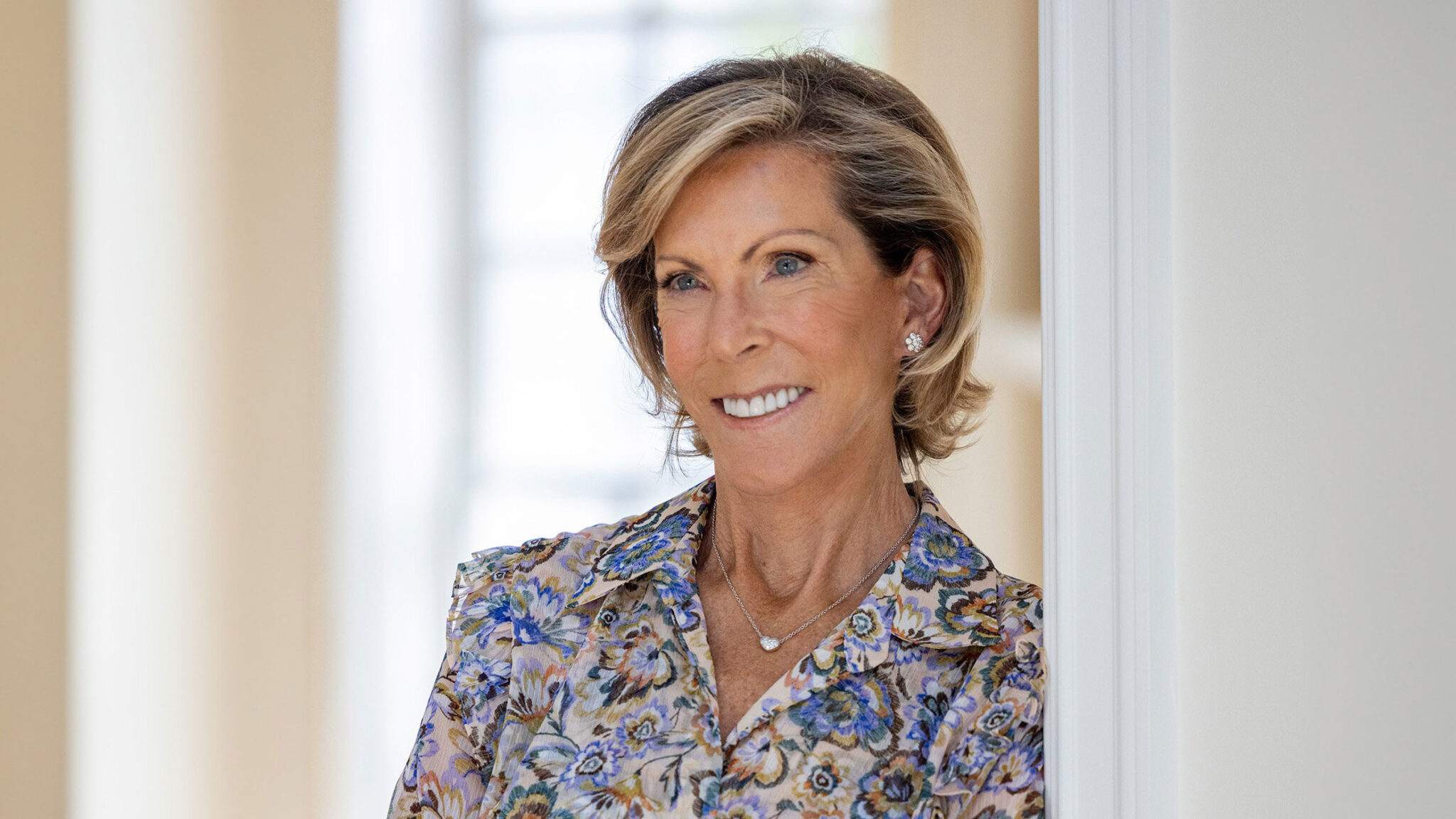
Kathy Giusti’s war on multiple myeloma is more than an example of the beat-the-reaper genre. Giusti, who was diagnosed with a smoldering multiple myeloma at age 37 in 1995, created a foundation that catalyzed the research that resulted in creation of the very treatments that ultimately saved her life.


Aiming to change the culture of research, the foundation Giusti started, the Multiple Myeloma Research Foundation, required researchers to share data and meet deadlines.
Giusti tells her story in “Fatal to Fearless: 12 Steps to Beating Cancer in a Broken Medical System.” In her blend of advice book, a crash course in cancer policy, and memoir, the memoir stands out as an extraordinary story of survival.
For patients and their caregivers, the book proposes a 12-step guide for staying afloat in what she describes as the “broken medical system” in the U.S.
Giusti calls her 12 steps a journey “from WTF to WTD.”
After getting a multiple myeloma diagnosis in 1996, Giusti started a journal she wasn’t sure she would be able to complete.
Said Giusti:
Back then, myeloma was so unbelievably fatal that the whole reason I’m able to write that personal narrative is because on my way out of Borders, where I was trying to learn everything I could about myeloma, I picked up that journal, because I was writing to our daughter Nicole.
That was really the start of it. I was writing to her, because it was the only way I could think of that she could remember me. I would just document everything we were doing together, and the places we were going, and anything that we were sharing.
And now here it is, 26 years later, and I have 26 journals, one for every year I never expected to live.
I really had to go back and read them, from cover to cover, in order to write the book. They really did give me a lot of insight into the toll that cancer really takes on a family when you’re trying to get through it. A whole different perspective.
Now Giusti has 26 volumes of journals, which she relied on in the writing of “Fatal to Fearless,” a story of good science, great timing, and all manner of luck.
Said Giusti:
Because I came from pharma, I actually had been through enough medical legal regulatory meetings to write beautiful newsletters and things like that that would not get me in trouble.
I was always writing like, okay, here’s the benefit, but here are the risks. I was so trained on that.
So, we were able to work with Celgene of thalidomide. Of course, Sol Barer was there back then, and we kept moving things off to Revlimid and Pomalyst.
And at the same time, there’s a beautiful story in the book about Julian Adams.
Again, the science is amazing, and sometimes, there’s just a tad of serendipity. Because on Velcade, when Julian was doing the very first trial, it was a phase I, it was all comers, and he happened to put a multiple myeloma patient into that phase I, and the patient went into a complete remission—and that changed everything.
At that point, Julian’s calling me, and, of course, we had a meeting—because we were always convening the myeloma community—we had a meeting ready to go and he just took it over.
They wrote the protocol, and we just saved so much time for patients. So, yeah, it was a really exciting time, and it kind of played to my strength, because I had been in pharma, so I loved that kind of work.
After her diagnosis, Giusti started the MMRF, which spearheaded the development of therapies, served on the National Cancer Advisory Board, and ran a science accelerator at Harvard Business School. And she raised two children, one of whom was born post-diagnosis.
Giusti acknowledges that she was extremely fortunate. At the time of diagnosis, she served as a pharmaceutical company executive at Searle Pharmaceuticals, a job that made her aware of how drugs are developed, how the academia operates, what advocacy can accomplish, the leadership drug development requires, and the nuts and bolts of drug regulation.
Giusti had excellent health insurance, a supportive husband, a supportive family, a network of friends. She even has an identical twin willing to donate bone marrow for a transplant.
When she started MMRF, Giusti had a business plan and demanded accountability from participating institutions. And she spearheaded building a tissue bank of bone-marrow samples and blood samples from patients with myeloma.
Said Giusti:
Where pharma started getting interested was realizing that we had a great biomarker. It’s so easy to follow a multiple myeloma patient in a clinical trial. All you have to do is follow our M spike. So, you could get trials done really quickly in myeloma. So, we were communicating that out.
Remember, the myeloma community back then was very small. There were like four to six academic centers actually working in myeloma. So, we did not have a loud voice at all.
Now, all of a sudden, our voice is getting louder. We’re spending a lot of time with NCI, down at FDA, we’re trying to build bridges. And I think the combination of knowing we had a biomarker, that novel drugs were starting to work, and the fact that it had such high unmet need meant that FDA would work with us to get these drugs approved.
I think that’s when pharma started saying, this is an interesting disease to take a look at.
In a 2008 profile of Giusti in The New Yorker, Jerome Groopman said her approach is “best suited to a disease such as myeloma, whose basic biology is at least partly understood.”
At the time, Kenneth Anderson, a myeloma researcher at Dana-Farber Cancer Institute (and Giusti’s physician) said to Groopman that the progress in developing treatments for the disease was in part due to MMRF.
“Myeloma now is a paradigm for new drug development, because of partnerships that occur between academics, large pharmaceutical companies, small biotech, the F.D.A., the National Cancer Institute, and foundations,” Anderson said at the time. “And, frankly, Giusti’s foundation has been a catalyst that created the urgency and awareness to make this progress possible.”
Though myeloma is still uncurable, the survival numbers are heading in the right direction.
Said Giusti:
Now, the five-year survival for myeloma—patients are living not the three years when I was diagnosed, but over 10 years. I mean, that is just a gift, because you think to yourself, “There’s always a lag in the data.”
I always say to people, if you’re going to get a cancer—and I’m so shocked to say this—but if you’re going to get one, you want to get one like myeloma, where there is just such an active pipeline and so much incredible progress.
It’s a reflection of the entire community. It’s never a situation where one person makes all that happen. It’s really just a lot of really good leaders, passionate about the patient and making a difference and being hungry to do it.
Myeloma had that. We really had it.
On March 15, for example, the FDA Oncologic Drugs Advisory Committee will review two multiple myeloma indications:
- Carvykti (ciltacabtagene autoleucel), suspension for intravenous infusion, submitted by Janssen Biotech Inc. The proposed indication for this product is for the treatment of adult patients with relapsed or refractory multiple myeloma, who have received at least one prior line of therapy, including a proteasome inhibitor, and an immunomodulatory agent, and are refractory to lenalidomide. Carvykti is a B-cell maturation antigen (BCMA)-directed genetically modified autologous T-cell immunotherapy.
- Abecma (idecabtagene vicleucel), suspension for intravenous infusion, submitted by Celgene Corp., a Bristol-Myers Squibb Co. The proposed indication is for the treatment of adult patients with relapsed or refractory multiple myeloma who have received an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody. Abecma is a B-cell maturation antigen (BCMA)-directed genetically modified autologous T-cell immunotherapy.
Giusti spoke with Paul Goldberg, editor and publisher of The Cancer Letter.
This conversation is also available as a video.
Paul Goldberg: Kathy, thank you again for finding the time to meet with me. Congratulations on your book.
Do you have a copy by any chance?
Kathy Giusti: I do.
Let’s show it. Just wave it in front of the screen.
KG: It’s a labor of love.
Yes, I have read it. I greatly enjoyed it. It’s three books in one, really. One is the memoir, and the other part is advice, and the third part is your conversations with our mutual friends.
KG: You’re so good. You picked up on the tapestry that we were trying to create, which was probably the hardest part of writing the book. There’s no point in sharing the stories from my memoir or personal narrative side unless they actually contribute to the what-to-dos.
I think we did it that way, because, to be honest with you, I don’t read a lot of what-to-do books. I like reading books that have stories and characters, and so, we thought this would be a much better way to go.
Well, the way you described it, it’s a progression from WTF to WTD.
KG: Exactly.
And it’s precisely that. My favorite part is the memoir, because it just tells an amazing story. I knew some of this, because—I don’t know if you know this—we were introduced by Ellen Stovall.
KG: Oh my gosh, isn’t that amazing?
Twenty-five years ago, give or take.
KG: She was such an incredible woman.
Well, she said the same about you, and I remember precisely what she said. She said, “Kathy Giusti somebody to know, because she does not get tired of telling people that bullshit does not cure cancer.”
KG: Well, that’s well said, I have to say. That’s very well said.
Speaking of the memoir, that part kind of explains it. I knew it in real time, but it’s not really visible prospectively. You kind of have to look back on what was going on, which is you had smoldering myeloma. You had maybe three or four years to find the cure? Plus, you also had IVF to have a kid. I knew some of this, but I didn’t know all of this. It’s an amazing story.
KG: Yes, it sounds a little frenetic; doesn’t it? On one hand, you’re trying not to die, and on the other hand, you’re trying to create a life. So, the two things going on at the same time were really quite something.
Now, the five-year survival for myeloma—patients are living not the three years when I was diagnosed, but over 10 years. I mean, that is just a gift.
But you know it all too well. Back then, myeloma was so unbelievably fatal that the whole reason I’m able to write that personal narrative is because on my way out of Borders, where I was trying to learn everything I could about myeloma, I picked up that journal, because I was writing to our daughter Nicole.
That was really the start of it. I was writing to her, because it was the only way I could think of that she could remember me. I would just document everything we were doing together, and the places we were going, and anything that we were sharing.
And now here it is, 26 years later, and I have 26 journals, one for every year I never expected to live.
I really had to go back and read them, from cover to cover, in order to write the book. They really did give me a lot of insight into the toll that cancer really takes on a family when you’re trying to get through it. A whole different perspective.
What was it like? Were there any surprises when you look back at 25 years of journals? I don’t know anybody who has 25 years of journals.
KG: I think that’s what makes the book so interesting, because when you’re reading the book, you’re realizing the shift I’m making that the very first journal has a sunflower on the front—it’s sitting here on my desk—and inside, and it’s really funny.
This was the first one, and inside this journal are still letters that I had written, things that I had saved for our daughter.
So, when you pick up a journal and everything starts falling out from 26 years ago, it’s pretty eye-opening.
And you can see how I’m writing in the first few journals. I’m assuming I’m dying. I mean, I’m just creating a plan to die, and all I want to do is build our family and leave my husband and Nicole really safe and happy. That was my goal.
And if I lived long enough that Nicole made it to kindergarten—that was a stretch goal.
And so, all of a sudden now, I’m hitting those milestones. I had my son and things are happening. And, as you know, the story starts to build out, the MMRF started working with the whole community, and next thing we knew, drugs were starting to surface like thalidomide and Velcade, and it was starting to change the entire landscape of myeloma.
And you can feel it as I’m writing, there’s a certain conference that I’m at, a myeloma conference, and I am realizing like, “Oh my God, we are finally making progress.”
And I start to write differently.
Maybe we should go back a little bit, because not only do you survive, but you also help develop the two drugs you later get as part of the transplant, which is Velcade and Revlimid, which did not exist at the time you had your high-risk smoldering myeloma—which is an astounding thing.
Lots of people wish for the cure, but you actually built the damned thing.
KG: Yes, it was such a fascinating time, but it shows you that when you have a rare cancer that is neglected, everybody that’s working on it, and again, it has no money, no funding; right?
So, everybody working on it feels the same: “If only we could get more eyes on this cancer, if only we could get more support.”
So, you really do build a community of academic centers, pharmaceutical companies, NCI, and I think that was the gift of starting the Multiple Myeloma Research Foundation was building that community and running the round tables and keeping all of us together, focused around one strategic plan.
But it was really thalidomide that came in and kind of changed the way we thought about myeloma. I write about that in the book. All of a sudden, a patient is requesting this drug for her husband and it didn’t work for him, but it worked for the next patient.
Yes. Beth [Wolmer Jacobson]; right?
KG: It was crazy. I mean, it was just an amazing time. Now, here’s Celgene, not able to communicate a lot to the patient community. They don’t have an approved drug.
And so, I’m starting the foundation, and I have a patient database, and at least I’m able to communicate out to the patient community what’s going on with thalidomide.
I’m not your typical patient. And I say that in the book. The things about me are I had a really good science background, and I had great insurance, and I had a phenomenal support system, and I had an identical twin. My whole point of writing the book was to say I had all of that, and I still got it wrong. I still messed up.
And again, because I came from pharma, I actually had been through enough medical legal regulatory meetings to write beautiful newsletters and things like that that would not get me in trouble.
I was always writing like, okay, here’s the benefit, but here are the risks. I was so trained on that.
So we were able to work with Celgene of thalidomide. Of course, Sol Barer was there back then, and we kept moving things off to Revlimid and Pomalyst.
And at the same time, there’s a beautiful story in the book about Julian Adams.
Again, the science is amazing, and sometimes, there’s just a tad of serendipity. Because on Velcade, when Julian was doing the very first trial, it was a phase I, it was all comers, and he happened to put a multiple myeloma patient into that phase I, and the patient went into a complete remission—and that changed everything.
At that point, Julian’s calling me, and, of course, we had a meeting—because we were always convening the myeloma community—we had a meeting ready to go and he just took it over.
They wrote the protocol, and we just saved so much time for patients. So, yeah, it was a really exciting time, and it kind of played to my strength, because I had been in pharma, so I loved that kind of work.
You were an executive with Searle.
KG: Right. And before that with Merck. So, that came naturally to me.
The things that didn’t necessarily come as naturally were more of the policy, or touchy feely, or the art of fundraising, which you have to learn pretty quickly.
Looking back at it, it was so logical that a lawyer could see it. I’m talking about Beth Wolmer Jacobson. She saw it and she called…
KG: [Bart] Barlogie.
I thought she called Judah Folkman first.
KG: Well, she might’ve called him first, because he was doing all the work in angiogenesis. And, ironically, we had done a roundtable with him as well, on that topic. So, he was doing some beautiful work in that and she picked up on it, and maybe then they got to Bart.
But why wasn’t this happening? Why weren’t doctors thinking of it? Because thalidomide is a pretty old drug; God help us.
KG: I know. I think people get stuck in a certain path. And it was really funny, in myeloma at that time, the focus was on stem cell transplant. Remember, that was still really new to multiple myeloma.
So, we were spending a lot of time. How successful is stem cell transplant? Who should be getting it? Should it be autologous? Should it be allogeneic? How do we get Medicare to cover it? That was one of the first projects I ever worked on—was trying to get stem cell transplant covered.
And then, on top of transplant, was vaccines.
So, this was really interesting. One of our first roundtables was on vaccine work in melanoma.
We wanted to transfer the knowledge of melanoma over to myeloma. So, we did it with NCI. This was back in 1998 or 1999. We were doing immunotherapy, and everybody was looking at DNA vaccines, dendritic cell vaccines.
So, the whole focus was in stem cell and vaccine.
Then when thalidomide emerged, it really did get everybody thinking outside the box, which was a good thing. Then, all of a sudden, now we’re shifting over to angiogenesis and novel drugs.
And again, every time this happens, we have to be smart and write an updated strategic plan to decide how are we spending our money. We’re putting less money now into vaccines and more money into novel therapies and things like that.
But why weren’t they really thinking? Why wasn’t pharma thinking that there was money to be made? Look at Celgene—sold for a pretty chunk of change.
KG: I think it’s because myeloma is a small, uncommon cancer. So, back then, a rare disease.
Where pharma started getting interested was realizing that we had a great biomarker. It’s so easy to follow a multiple myeloma patient in a clinical trial. All you have to do is follow our M spike. So, you could get trials done really quickly in myeloma. So, we were communicating that out.
Remember, the myeloma community back then was very small. There were like four to six academic centers actually working in myeloma. So, we did not have a loud voice at all.
Now, all of a sudden, our voice is getting louder. We’re spending a lot of time with NCI, down at FDA, we’re trying to build bridges. And I think the combination of knowing we had a biomarker, that novel drugs were starting to work, and the fact that it had such high unmet need meant that FDA would work with us to get these drugs approved.
I think that’s when pharma started saying, this is an interesting disease to take a look at.
This was before Pazdur, even.
KG: Yeah.
But Pazdur, I’m sure, helped.
KG: Oh, he was amazing. I mean, I have to say one of the best partners we had in the field of multiple myeloma was FDA. Absolutely.
And he comes in around year 2000. So, by then, a lot of the work’s already done, but there’s a lot to do.
KG: Yes, because it’s around that time that you’re starting to see Revlimid, and Velcade is just starting to emerge. And fortunately, Sol Barer was also committed to keeping Pomalyst in the pipeline at the same time, too. So, there was a lot going on.
And, of course, we were still looking at stem cell transplant.
And back then, there was still a lot of discussion of how to do it. Do you do two transplants? Do you do one transplant, see how the patient does, and then consider doing a second? Do you dare do allotransplant, or is it still too fatal? So, there’s a lot of work going on in that space too.
The most astounding thing about the story is not only do you—actually, I’m going to quote Jerry Groopman’s profile of you from, I think [2008], which was quite beautiful. He kind of wrote that, here’s a new kind of patient who is trying to buy their own cure, which is what you were doing.
KG: I really was.
I can’t say I did it intentionally. I just did it, because I was very fortunate that early on I was still working at Searle and, ironically, they were doing a United Way campaign, and all of the employees wanted to support the United Way campaign and support myeloma research.
So, it shifted, and then, thank goodness, my identical twin was an attorney, and that’s what got the foundation off the ground. So, it wasn’t like I was saying, “Oh, my gosh, I’m just going to go start a foundation and save my life.”
But once we could start funding research, I felt like if I could bring more scientists into the fold, if I just got that much done, maybe I would see Nicole to kindergarten.
Maybe I would beat the three years and get three-and-a half, or four, or something, and do a little bit better. That was all I was thinking. And then, all of a sudden, this foundation starts to take on a life of its own.
So, not only do you have this drive and the vision, but you also have an identical twin, which is something that comes into play because of the stem cell transplant.
KG: Yes, I think that part’s really important, because I’m not your typical patient. And I say that in the book. The things about me are I had a really good science background, and I had great insurance, and I had a phenomenal support system, and I had an identical twin.
My whole point of writing the book was to say I had all of that, and I still got it wrong. I still messed up.
That was much later. We’ll get to that.
KG: But I mean, I even messed up along the way. And so, when you go back and read it, you’re like, how can we possibly expect patients who don’t live in this world that I do to be able to figure this craziness out? It’s a challenge.
You quote Cliff [Hudis]: “The American healthcare system is not a system.”
KG: Right? It’s a disaster. It’s a disaster. It’s absolutely a disaster.
And I think my three biggest issues with the system are:
Number one, it is so fragmented and it is left to the patient to integrate it. So, you get a cancer diagnosis, it may come in from your internist or primary care or whomever, a suspicion, and now you’ve got to figure out medical oncologist, surgical oncologist, pathologist, radiation oncologist. Your head is spinning, and then you’ve got to put all those people together.
And I think the second piece is that now, the science moves so fast that you have to try to stay on top of the science in making your decisions. And the doctor only has 16 minutes with you, on average.
So, it’s you and your partner—it could be your son, your daughter, your husband, your wife—you are now really trying to figure out these incredibly challenging decisions and reading lots of high science that you don’t understand. And that’s hugely frustrating.
And then, the third is the cost.
It’s so easy to get stuck with out-of-pocket. It’s so easy to mess up on the reimbursement side. And so, you’re constantly having to be on with insurance companies, and it just creates stress.
And I think that’s another reason why I wrote it was like, “Just be aware of these things and find people to help you with it, because if you take it all on yourself, it will wear you down.”
Plus you have all these friends too. What is it? “The Eight,” as you described.
KG: The Eight. I still have The Eight, thank God.
That’s another thing I say, who has eight friends willing to help them? I’m an extreme. Not everybody has that. It doesn’t matter. You don’t have to have eight.
My point is, when it gets to knowing what your needs and wants are, if you can find one or two people that will help you, and you work with them wisely, you will be okay. It will help you so much.
I guess that’s an artifact of a retroactive look of every memoir—everything works out.
KG: I know.
Although you really can tell, by the time I’m getting to the end of the book, I’m like, “Jeez, I screwed up.”
So, I really do feel like it ends fine, but it probably could have ended better, if I had been more on my game, or watching what was going on around me more.
Where do you think you screwed up? You don’t screw up very much, but at the end of the book, there is a mishap that you see as kind of your own. Can we talk about that?
KG: The biggest takeaway for me was I was always focused on cancer from the patient’s perspective, and I was always focused on it from the business perspective. How are we going to drive the MMRF forward? How are we going to make more progress? How will we see more drugs? How will we save the next life?
And I was always petrified that I was going to relapse. I still am. It’s not like I go to Dana-Farber and think, “Oh, I’m cured.” I don’t. I am always wondering what’s next when a patient relapses.
And I think the book was more eye-opening, for me, reading about everything that the people around me were sacrificing.
So, the examples I give in the book are, I’m heading out for a stem cell transplant. And that was happening in 2006. And just to get me through the Cytoxan, the chemotherapy, harvest the stem cells, I was doing it with my sister.
I mean, she was going through a really tough time. She was going through a divorce. And all I could think about was did she get her Neupogen shots? How are her stem cells doing? How is she going to meet me at Dana-Farber? She had three little ones at home—how are we handling babysitters? She had so much on her plate.
And the same thing for my husband. Now, I’m gone. I’m gone for three to four weeks by myself. And same thing for our children. Nicole was in sixth grade, in middle school, and now, I’m gone. And she’s petrified. You can tell she’s scared.
The science is amazing, and sometimes, there’s just a tad of serendipity
I write about this in the book. She felt like she had to be the perfect child. God forbid she get me sick, she get me worried, she concerned me for any reason whatsoever. She just felt she had to be so perfect.
I think, looking back on that, it was a really tough time when I was not paying attention to the toll it was taking on everyone around me. And then you get through it, and everybody’s looking at you like, “Okay, we’re done. This has been a lot of time, a lot of energy. We all worked. Everybody was working,” that was my caregiver.
And now, I’m depressed. I’m feeling like I can’t function in this world. I don’t know what to do with myself. And the first person I call, again, is my sister. And I drag her back up to work with me again.
So, you read the book, and you’re like, “Oh my God, I really needed a lot of people.” My friends were constantly coming over and making food, and things like this.
I handled my medical pretty well, because I didn’t feel like anybody else could handle the medical as well as I could. I was going to study it, know it, be on it, but it was the other things that I failed to pay attention to. And I think it did take a toll on people around me. A big toll.
Also, you described the breast cancer episode.
KG: The breast cancer was so different, because in myeloma, our son, David was only in third grade, and Nicole was in middle school.
So, for him, he doesn’t really remember a lot of it. There’s certain things he does, but a lot of it, he was just there to keep me laughing and keep me company—play battleship with me, play games with me, do puzzles, whatever, while I was home so sick after the transplant.
By the time I got to breast cancer, now he’s an adult, and he is worried, because he hasn’t been through this before in a way that he remembers it, and he’s like, “This is brutal.”
And now, I’m going in for surgery, and you’re describing the surgery, and you think you’re going to get through it quickly. Of course, he took off work—he and Nicole, everybody—took off work to get me through the surgery and be home.
He was going to cook, walk the dogs, do everything. And sure enough, they’re all home, took off work.
I got COVID. I couldn’t go in for the surgery. It got delayed weeks, and now, he feels horrible. He can’t take off work again. He is desperately trying to; he’s getting home on all the weekends.
At a certain point, Nicole ended up having to move out West, and David was by my side with his girlfriend. So, you switch, and now, he is doing a fair amount of the caregiving. And he’s watching, and I am getting really sick with infections. There’s a point in time where both Nicole and David are home. And I realize, “I think I have sepsis, I am so sick.”
It’s Memorial Day weekend, and they have to handle me. And thank God they’re really rational and smart, and we got me back to the hospital, got me there in time, and it was brutal.
It’s hard to put your kids through that. It’s a lot. It was a holiday weekend. They came, they come home thinking, “We’re going to have great time. We’re so glad we’re not in the city right now.” And then all of a sudden, “Oh, nope, we’re back in the city at Mt. Sinai.”
Oh my god, “Mom has sepsis.”
KG: “Mom is super sick.”
I think just seeing all that over and over again—and it wasn’t even just me. You have to realize, for our kids, their grandmother had melanoma. So, they watched that. She was always showing up with stitches all over her face, her scalp. And then, my sister ends up with stage 3 breast cancer.
So, our kids have seen a lot of illness, a lot of illness.
Plus, your father-in-Law had—
KG: Yeah, they never met him. He died so young. But they knew that he had died of renal cell carcinoma.
I mean, it’s really interesting. You know how your kids have to put together the charts of the family. Here’s my mom, here’s my dad, here’s the grandparents. And after doing this, we kept going through and saying, “Well, what happened to that one? What happened to that one?”
Finally at the end they’re like, “We have the worst genes. These are horrible genes.”
And since my sister is an identical twin—and she has three children, all the cousins—they feel the same way. They’re like, “We all are screwed. All five of us have really lousy genes.”
That’s why it’s funny, even with these new articles that come out on the increased incidence of cancer in young people—colorectal, cervical—I’m talking to my kids about this.
I write this in the book: Get your kids to a really good primary care doctor. They need to be seen. They need to get physicals. They don’t think about it, but they have to have a place to go.
Absolutely. A very interesting piece, for me, was looking for people I know. It’s kind of like a modified “Washington read.” The “Washington read” is where you just check whether you’re in there. I’m not in there, but I was looking for people I know, and it was nice to see them, and it was nice to see how you describe them.
I think one person that has a place of honor in this book is Ken Anderson.
KG: Yes, he was a very—and still is—an incredible clinician, and there for his patients 24/7. I mean, the man worked tirelessly. I love the sections in the book where I’m talking about my sister Karen—my identical twin—and I coming up there. And we really felt like identical twins were something that should be studied.
For doctors, they’re taught do no harm. So, we had to honestly keep going back to Ken and saying, “You don’t understand. We are raising our hand. We’re going to be really upset if you don’t take us up on this offer. We really want to be doing this.”
It took everything he had, because now, he’s doing bone marrow aspirates with my sister, who is a healthy subject.
But the work was really productive, and it told us a lot—what genes are turned on and off in each other; her immune system at that point was better than my immune system.
So, there was just a lot of really good information we were finding. And as you could sense, the beauty of Ken Anderson is he’s a great clinician, but he’s also a great translational doctor.
It was true bench-to-bedside at Dana-Farber. They’re doing genome sequencing, and they’re doing gene expression profiling, and they’re learning everything they can, and then they’re tying that back to the clinic. It’s really important.
Plus you were one of the first people to get PCR testing.
KG: I was very fortunate in that, because I was a t(4;14), and Ken knew anecdotally that Velcade was a nice drug for t(4;14).
At that point, remember, t(4;14) is really high risk. They’re still high risk, but there’s not as much concern about it as there used to be. And because of that, Ken really did battle to try to get me on that soon.
So, you set up the MMRF, and you take a role in development of a bunch of drugs. Also, really, the needle is moved on multiple myeloma.
Do you have the numbers on that?
KG: Well, at this point, there are over 15 drugs approved in multiple myeloma.
As you remember, there was a flurry of activity that happened moving from thalidomide to Revlimid to Velcade and building out the proteasome inhibitor category.
So, we were all on triplet therapy for quite a period of time. I remember Ken had a great SPORE grant that he was doing to just kind of say, “How are we combining these classes of drugs and how do we make them the best that they can be?”
So, we learned a tremendous amount about that information. We spent a lot of time, by the way, on all of that work, trying to make sure we understood it really well, and also how it worked with stem cell transplant.
Then, I think, when daratumumab came along, that was really fascinating to understand, because now you’re looking at antibodies, and you’re also watching how long it takes to get a really, really good drug like daratumumab into the hands of all patients.
Because, again, remember, everything is done in relapse/refractory patients. You’re trying to figure out combination approaches. And now, in today’s world, most doctors will tell you if you have myeloma, to go ahead and start with a quad therapy including daratumumab.
So, that moved us into the antibody space. And now, as you know, we’re in the next revolution of multiple myeloma, which is immunotherapy.
I feel like this time, right now, is reminding me of the same time we had when we were sitting there with stem cell transplant and the triplet, and we’re trying to figure out what do we do to make sure that we’re getting patients into as deep a response as we possibly can.
There was a lot of work going on there. If you remember, it’s hard. Pharma looks at their own drugs. It’s not so easy to do tons and tons of trials looking at sequencing, dosing, all those kinds of things. So, unfortunately for the patient, we don’t get that information that fast.
Now, with immunotherapy, it’s kind of the same thing, where there’s a multitude of drugs, and now, we’re trying to figure out how to use them.
And just like stem cell transplant took a long time to get out to the community—because it’s hard to do and you didn’t want to mess with that if you were out at a community center—it’s the same thing with immunotherapy.
We know we should move it to the community. Everybody wants to move it to the community, but these drugs are toxic. They’re hard to take and hard to deliver. As a result, now we’re in another situation, again, where it feels a little unfair that the patients that it can afford and are at the academic centers are more likely to get these immunotherapies than the patients sitting at the community centers.
That tells you a lot about myeloma, which skews older, male, and African American, that one of the biggest jobs we have as a community is making sure that treatment is fair and that we have full access for all patients.
I think that’s really one of the things that the MMRF is 100% dedicated to right now, is saying, “There are so many really good drugs. I even think between the drugs that we have approved and the ones that are in the pipeline right now and in trials, we probably have some curative approaches. But we have to speed the process of making them less toxic, knowing how to combine them, knowing how to sequence them, having a real clear journey for the patient and getting things to the community.”
It’s a big job, but it’s important.
If you want to get some of these tough-to-take therapeutics, first of all, you may not be able to get it at a community center, because they’re doing the trials and they’re doing a lot of the work at the academic centers, because they have to.
Over time, I think everybody finds a way to make it easier and it will shift out to the community. But it takes so long. So many times we wrote the marketing plan for the MMRF, and we were always trying to create a hub-and-spoke environment where you’re really creating this netting between the academic centers and the community.
I think that, over time, that might happen as the NCI, for example, says to the NCI cancer centers, “You don’t get your cancer center grants unless you are treating all patients and all kinds of patients.”
I think that is forcing some of the cancer centers to really open up their doors and create better relationships out in the community. You have to bring the drugs and the trials to the patient.
There’s just no way with people working and trying to get through this that they possibly can do it and get through tolerating tough drugs. It can save their life.
I mean, I think that’s why I love the whole thing of immunotherapy, because I do feel like I benefited from that with my twin sister, and then when I relapsed, doing donor lymphocyte infusion. So, I feel like there’s a lot to what’s going on here.
It’s almost like at the level where a complete agnostic like me wonders whether somebody is looking after you.
KG: We can only hope. I don’t know.
That’s not a question, I withdraw my question.
So, I guess one area we didn’t yet cover was the accelerator you were running at Harvard.
KG: Yes. I loved that job. It’s just so coincidental that here I was, helping and caring for my sister, who had stage 3 breast cancer, which is tough and really scary. And she’s still scared. And she’s a single mom trying to figure out her insurance.
So, that’s why I love her as a character in the book, because she had different issues than me, and they’re real issues and they were incredibly important.
So, I was working with her and trying to get her to the right doctor. She decided on MSK, and at the same time I was working with my mom who had melanoma and I had her at UPenn, and then I’m being treated at Dana-Farber.
So, I’m just doing the circuit from one center to the next. And we all had community centers we were working with, too.
It’s just these academic centers where our team approach of have an academic advisor and have a community center that can work with you. And then, all of a sudden, this call comes in from the dean of Harvard Business School saying, “We love your model. We love what you’ve done at the MMRF and Robert Kraft wants to work on precision medicine. Would you come up here and run a program around precision medicine across all cancers and diseases?”
I thought, “This is probably meant to be, because why else would this be happening right now?”
It was just an amazing time to work directly for the dean, and Robert Kraft was a true learning experience for me. I was blown away at how collaborative people are, and this is what I found at the MMRF, too.
If you can lead with a strong strategic plan and you can bring everybody in, from all facets of the community to chime in, to have a point of view—you’re never going to all agree, but you have to work through it, and reach some level of consensus, and keep moving forward.
If you take that same concept and go up to Harvard and say, “Look, there’s a lot that myeloma can learn from pancreatic cancer and brain tumors and breast cancer. And, by the way, there’s a lot that Alzheimer’s can learn from cancer.”
So, looking at it that way, I would bring the brightest minds up onto campus with my co-chair, Richard Hamermesh, and we would just make them think like business people:
Follow the money, figure out what the incentives are, what are you doing here? We really trained them all to think differently.
I love the fact that we have left behind a full playbook for anybody looking to start a foundation, because I get a lot of calls like that, and I always say, “Go to the Kraft Accelerator site first. You’ll find every article I’ve ever written with Richard, every case study we used, and you’ll find the MMRF strategic plan I was writing at the same time. It’ll tell you how to do it.”
And that was my playbook for foundation leaders. I felt like this is really good, at least they have a place to go.
Thousands of people have used it, which is great, but then I basically had to finish there after COVID, and it was like, “We don’t have a playbook for patients, we just don’t have one.”
So, that’s when I knew it was time to start doing that.
That’s your book.
KG: That’s the book.
That’s really why I wrote it. I felt like, I knew how scared I was. And the irony of it all is now, I sit down to write the book, I’m going through all the journals, I’m getting ready, I’ve decided that it’s going to be Harper Collins that works on the book with me, I’m getting all my thoughts together. And then I get breast cancer.
I was just reminded like, “Oh my God, this system is still the same broken system. It’s just different.”
With myeloma, I couldn’t find any articles. Nobody had been working on it, and we didn’t have the internet. So, I’m sitting on the floor of Borders bookstore, just hoping I can find something I understand on the topic in breast cancer.
And I write this in the book too—I’m sitting in the car going, “Oh God,” looking at my husband going, “It’s early, it’s fine. Let me just Google a little bit here.”
I get 2 billion hits. Two billion. What am I going to do with that?
So, the world has changed so much, in terms of the responsibility on the patient, that it’s just crazy.
So, I mean, I felt it back then when I got diagnosed with myeloma, but now, you are the curator of your own information to save your own life.
And that’s why the first parts of the book are, “Get on your game. Don’t go down the rabbit holes, don’t get distracted. Go to the best sites, get to the best doctors and stay focused.”
It’s really the most important part from the moment you get diagnosed.
Remember, in today’s world, we get diagnosed on our portals, before the doctor tells us. At least with myeloma, I had this lovely internist softly telling me what was happening with myeloma and then moving over to my heme/onc.
In this situation, today, so many patients are reading their portal and realizing they have cancer, and the doctor can’t get to them. So, they’re immediately going on to Google.
I don’t know how informed decision-making is being done in breast cancer. That’s got to be extraordinarily difficult.
KG: It’s so hard.
I always thought myeloma was so confusing, because it’s a blood cancer, but it affects the kidneys and the bones, and the name doesn’t make sense and it’s just a confusing cancer.
And I thought, “Oh, breast cancer will be so much more logical.”
But there’s so many types of breast cancer and so many approaches, and again, it’s really hard to get consensus, so many of the decisions are left with the patient.
In my situation, I took a really aggressive approach. I’m sure there are many people that would say doing a double mastectomy for such early breast cancer was crazy. But I also knew if I did that, I wouldn’t have to do radiation and chemo and I would be done.
For me, I was like, “Okay, if I can be done with cancer in six months after I’ve tormented my family for all these years, I’m out.”
Little did I know that in solid tumors, the risk of infection goes way up and I was still battling 18 months later.
So, the different cancers, they’re all tough and they all have different stories, but the one thing they all have in common is find them early, because you’re going to have a lot more options, and it’s going to be a lot easier on everybody.
Even when you look at the caregiver studies, the patients that are diagnosed early stage are doing great and so is their caregiver. It’s when you get to later stages that now, the patient is really sick, the caregiver has to step in to help with decisions and taking care of the patient.
They’re missing work, they’re missing their livelihood and stress just bubbles.
Plus you do a lot of individual counseling work. I know that every time anybody I know gets myeloma, I send them your way and I just give them your cell phone number.
KG: It’s funny. I’m always happy to help, because I know how I felt when I got the diagnosis and I didn’t know where to turn. I think that was another reason I wrote the book. I finish these calls with patients—I typically follow the same routine of asking them specific questions and kind of going through where they were.
I felt like that was why I needed to do the book, because at the end of the call, they would always look at me and go, “Oh my God, in 20 minutes with you, you just saved me five months of pure aggravation. I understand it so much better and I finally have some hope.”
I thought to myself, “This is not a sustainable model of me doing this. It’s just not going to work, and I’m not going to help everybody if I do it this way.” And I thought, “If I can put it all in writing, that would be a gift for the patients and the doctors who serve them and the caregivers, and it would make life a heck of a lot better for everybody.”
Then, as you know, you don’t have to buy the book. I put the 12 steps on my website, so anybody can have them, and I’ll keep building that site out. People can just go to my site if they need it.
Oh, they should buy your book. Come on.
KG: Well, the book is a nice companion so you don’t feel so alone. You’ll read it and be like, “Oh God, I get that. I understand how she was feeling.”
It’s kind of like you read my story, but you find your own cure. I’m just jogging your memory to think, “Did I do that? Should I do that?” I’m just like that voice in the back of your head.
No, it’s fantastic. And this is a really difficult question: Is there anything I forgot to ask?
KG: You covered a lot actually. You really did.
The only other piece, and this was something that I saw on The Cancer Letter (The Cancer Letter, Jan. 5, 2024) that was amazing, and I’m doing a piece on this. So, two people I interviewed in the book where Arif Kamal at ACS and Karen Knudsen at ACS; right?
I don’t normally interview two people from one organization, but I started with Karen, and she loves him, and, basically, he runs the whole navigation program for ACS. Then, I saw your whole piece on Medicare reimbursement and the two of them were interviewed.
So, you spurred me on to write back to them and say, “Guys, I don’t fully understand this. What’s going on with it?”
So, Arif started explaining it to me and explaining that ACS is doing some of the training. They told me that one of their biggest problems is people don’t know that the reimbursement is happening.
The community hospitals, where they could be getting navigators on board, don’t know to do it, and the patients don’t know to ask for it. I did say to him, “My whole point of doing the book is, I am your navigator. I’m just there to help navigate you through the system.”
That’s why I spoke to Arif and said, “If there’s anything I can do to help you with this and let people know that it’s really important.”
I do agree—one of the short-term solutions to the mess of our broken medical system is getting more navigation in, because I don’t know how else you solve these really big problems unless you can bring in navigators that look like the patient.
Just so you know, we have full-time nurse navigators that come out of the major cancer centers. These are really, really smart ladies, and they will work with a patient from the beginning, from the moment of diagnosis, until the end. They know every center, every doctor, every study.
Yet, the call center, in my mind, is underutilized. You’d be shocked. You would be shocked to know it takes a long time for a patient to find a patient foundation. A long time. Often, it’s like one-third of the patients ever find them. Even then, they’re scared to give their email because of privacy issues.
And yet these foundations—Longevity, PanCan, MMRF, ACS—these are really well-run organizations with a wealth of information for a patient.
So, when they get stuck, there are places for them to go—not for every cancer, but for a lot of them. They’ve just got to pick up the phone and call. Just call. They’d be surprised at all the things that these groups offer.
I’m always surprised—the doctors are so busy. They don’t tell the patient that there is an organization out there. It would be such a gift.
I said that to Arif, “It’s great if the community hospitals and everybody can put together navigation programs and bring in trained navigators at the hospitals. But I pray that they do a much better job of explaining to the patient that there are disease-specific foundations out there that are really well-run.”
If you’re questioning it, go to Charity Navigator. You can see if they have a good rating, and if they’ve done well. It’s not hard.
Well, some of it is also politics. I think some of the groups should be politicized. One of my favorites on that score is the National Breast Cancer Coalition, because that’s a model of a group that became very political—in a good way.
KG: This is where, again, you have to decide. As an organization, you can’t do everything. That’s why writing the strategic plan and being such a business-minded group is so important. You can’t do everything because you don’t always have the money to do everything. So, it can vary.
You can be a great organization focused on policy and really changing the world. I think Ellen Sigal does this really well, too. There’s different people that take on these jobs, but Ellen would be the first to tell you she’s not going to sit there and do what I did—literally living and breathing the research and drug development side.
But that was my love, and myeloma needed new drugs. So, it was quite an effective way to go. But the organizations are all different, but there are so many resources if patients know about them. And again, depending on what matters to you—whether it’s a policy issue or finding a drug or you have side effects or you don’t know what doctor to go to—you can find help.
Actually, I do realize one question I did not ask is the survivals. Maybe that’s a good way to conclude.
How have the numbers changed?
KG: Now, the five-year survival for myeloma—patients are living not the three years when I was diagnosed, but over 10 years. I mean, that is just a gift, because you think to yourself, “There’s always a lag in the data.” And with the pipeline of new drugs that we still have available, it’s just going so incredibly well.
I always say to people, if you’re going to get a cancer—and I’m so shocked to say this—but if you’re going to get one, you want to get one like myeloma, where there is just such an active pipeline and so much incredible progress.
It’s a reflection of the entire community. It’s never a situation where one person makes all that happen. It’s really just a lot of really good leaders, passionate about the patient and making a difference and being hungry to do it.
Myeloma had that. We really had it.
Well, thank you very much.
KG: Thank you. It’s always fun talking with you.