This story is part of The Cancer Letter’s ongoing coverage of COVID-19’s impact on oncology. A full list of our coverage, as well as the latest meeting cancellations, is available here.
The NCI Board of Scientific Advisors has approved concepts for an RFA and an RFP to support research in serological testing.
The plan presented to BSA May 12 is intended to distribute $306 million in new money the institute received “to develop, validate, improve, and implement serological testing and associated technologies” under the Paycheck Protection Program and Health Care Enhancement Act (P.L. 116-139).
The bill, which gives NCI new funds for the serology effort, was signed on April 24. The institute has been working rapidly to engineer the complex research plan.
The org chart—a hub-and-spoke structure reminiscent of those NCI used to manage large collaborations during the peak Moonshot years—calls for engaging NCI constituencies, but also outreach beyond oncology, to explore collaborations with immunologists and microbiologists.
“I, for one, will be very surprised and very sad if we don’t get some new cancer antibody work out of this, because it’s just so natural,” NCI Director Ned Sharpless said in a BSA discussion of the COVID-19 serology concepts.
The concepts incorporate insights from the institute’s discussions with leadership of cancer centers, reflecting the notion that the COVID-19 pandemic has demonstrated that there has been a convergence of research in oncology, immunology, and infectious diseases (The Cancer Letter, April 24, 2020).
The institute’s serology push comes at a time when basic science labs at cancer centers remain closed amid the coronavirus pandemic. Given how quickly the program is expected to move, those vying for grants would be wise to stay vigilant.
On May 14, NCI published a Request for Information, which would remain open for 10 days. “Leaving it open for only 10 days isn’t optimal, but necessary in order to stay within the time frame that we were required to work,” Dinah Singer, NCI Deputy Director for Scientific Strategy and Development and one of the principal architects of the program, said at the BSA presentation.
The RFA and RFP are expected next month.
NCI role in establishing standards for SARS-CoV-2 assays
In another development related to the COVID-19 pandemic, NCI’s Frederick National Laboratory for Cancer Research plays a key role in establishing criteria for evaluation of serology tests, and FDA is now starting to use this template to evaluate tests that have been allowed on the market under FDA’s Emergency Use Authorizations.
“Last Monday, news hit about the FDA’s revised policy on antibody tests for commercial tests of manufacturers related to the EUAs, and providing specific clinical performance expectations for those tests,” Sharpless said at the BSA meeting.
“It’s a little bit hard to understand exactly what the FDA is doing there, because they couch their announcement in the careful argot of the FDA. But since I’m fluent in FDA, let me translate. The announcement says the FDA is ending enforcement discretion for these mini serological tests currently on the market.
“Manufacturers of these devices have 10 days to come in with an application to the FDA, or an EUA—or else, meaning that they will presumably be asked to pull their test from the market. The reason they can now take this much stricter approach, is because they have a pretty good idea of which tests work and which ones don’t.
“And they also have confidence that a few manufacturers are now producing testing capacity in large supply. And these tests are becoming more generally available. And therefore they can be more demanding that the manufacturers meet a certain quality standard. And the reason they can be more picky about the tests and the reason they have confidence in some of these tests is in part, in large part, because of the work being done at the National Cancer Institute.
“At Frederick National Lab, we’ve been using our long-standing expertise in serological testing, on behalf of the federal government, in concert with the CDC and BARDA and academic partners who’ve been crucial in this as well.
“And we’ve been doing performance testing for the FDA. And have provided high-quality, dispassionate evidence that serological testing can work, that there are high quality assays—and in particular, these assays can be made widely available for the American consumer. The FDA has made our results available on their website, and we published a new post on NCI’s Cancer Currents blog, that delves a bit deeper into this topic overall. And I encourage you to read that post, if you’re interested in this.
“Our work continues there on behalf of the FDA and other parts of the federal government. It’s been a really successful and exciting partnership across the federal government to identify an important testing modality, a benefit to the public health. And I think we’ll take on a large, important role in vaccine development as well, as that gets going.”
RFA and RFP concepts in COVID-19 serology research
NCI COVID-19 Pandemic Urgent RFA Concept Request
In light of the emergence of SARS-CoV-2, and the urgent need to mitigate the pathogen’s spread, in the most recent COVID-19 supplemental appropriation (Paycheck Protection Program and Health Care Enhancement Act (P.L. 116-139)), the National Cancer Institute (NCI) received $306 million to develop, validate, improve, and implement serological testing and associated technologies for the purposes specified under the Act.
Working in collaboration with the National Institute of Allergy and Infectious Disease (NIAID), NCI plans to use a significant portion of the funds to establish a collaborative network focused on characterizing the immune responses elicited by this infection, understanding the mechanisms driving serological, humoral and cellular immune responses, and determining the serological correlates with disease pathogenesis and protection against future infection.
Specifically, the NCI plans to establish a Serological Sciences Network by funding 4-8 Serological Sciences Centers of Excellence, using the U54 mechanism. In addition, plans are to fund 5-10 Serological Sciences projects using the UO1 mechanism. These Centers and projects will work collaboratively with the Frederick National Laboratory’s Vaccine, Immunity and Cancer Program, thereby forming the Serological Sciences Network. A coordinating center for the Network is also planned.
Funding is estimated to be approximately $2 million TC per year per U54 Center for up to 5 years and $500K TC per year for UO1 projects with funding to begin by the end of FY 2020 or early in FY 2021.
To expedite the funding of the Centers of Excellence in Serological Sciences, plans are to issue the FOA by the end of June, or earlier if possible.
Also, using the emergency FOA authorization which allows great flexibility throughout the process, the application receipt date would be July 30. Primary peer review will be expedited by the NCI Division of Extramural Activities to ensure that second level review by the National Cancer Advisory Board occurs at its September 2020 scheduled meeting.
NCI COVID-19 Urgent RFP Concept
In light of the emergence of the novel coronavirus, SARS-CoV-2, and the urgent need to mitigate the pathogen’s spread, the National Cancer Institute (NCI) and the National Institute of Allergy and Infectious Disease (NIAID) plan to establish a collaborative Network of Excellence to develop serological assays of high specificity and sensitivity for rapid deployment to test for SARS-CoV2 induced immune responses.
To address these critical gaps, we plan to work with key stakeholders—FDA, academic and commercial partners with interest and expertise in immune assay development – to standardize, harmonize and expand capacity for serological antibody testing for SARS-CoV-2. NCI plans to establish Capacity Building Centers focused on development and expansion of serological testing capacity and practice. These Centers will serve as a critical component of a Serological Sciences Network in Response to SARS-CoV-2 Infection. Funding is estimated to be approximately $3 million TC per year for each Center. In addition to the Capacity Building Centers, the Network will include the FNL serology laboratory, the Serological Sciences Centers of Excellence and the Serological Sciences projects.
The Capacity Building Centers will address unmet needs in serological: 1) standardization, 2) assay development and 3) availability of SARS-CoV-2 testing to identify those who may have been exposed to the virus. Utilizing validated EUA SARS-CoV-2 serological assays with evidence of high specificity, sensitivity and reproducibility, will increase not only the national testing capacity, but also enable comparisons of data across different studies.
Therefore, it will facilitate an understanding of natural history of the infection, vaccine development and implementation of new vaccine candidates. This work will be conducted in partnership with the other components of the Serological Sciences Network to develop and make available reagents and standards to the serology community once generated and qualified.
Sharpless on serology research program:
A transcript of Sharpless’s and Singer’s presentations of the serology program follows:
Sharpless: It seems as though the word “serology” has suddenly, and understandably, become a household word in the United States. Congress appreciates the high-quality work that’s been provided by the NCI on this topic, and also knows how important understanding the science related to serology is and will be, for our efforts against the coronavirus pandemic.
And Congress really seems to appreciate one clear fact, which is that the NCI—with our capabilities of Frederick National Lab and our world class expertise in virology, and our extensive networks for clinical research—that given these factors, the NCI is best positioned to lead this much-needed serology research effort, and they’ve asked us to do that.
In this regard, Congress has passed four supplemental spending packages, providing emergency funding from the government to support the economy and small businesses, as well as to preserve critical operations in places like hospitals.
The fourth supplement was called the Paycheck Protection Program and Health Care Enhancement Act, and passed last month and was signed into law on April 24. This supplemental funding bill includes a significant new appropriation of funds to the National Cancer Institute—specifically, $306 million to develop, validate, improve, and implement serological testing and associated technologies.
Working closely with the National Institute of Allergy and Infectious Diseases, we have begun planning how to use these funds for the public benefit, and that discussion has already led to a concept that Dinah will present later today. But let me make first two very important points about these new monies.
First, know your funding is distinct from our annual appropriation. We are not being asked by Congress to work on coronavirus serology research with monies intended for cancer research. But rather, we are being provided here with extra new money for serologic research.
And second, the NCI does do cancer research and cancer is our clear priority. But it should be obvious to all here why progress against the pandemic will have important implications for cancer patients. So, better serology will help all patients, especially those with cancer. To be clear, this legislation is not specific to cancer.
We do not envision that this money will specifically fund serology research solely in patients with cancer. We will use it to just fund serology research. It is unusual, but it’s not unheard of for the NCI to focus so strongly in an area that’s not directly cancer research.
I think the last time this happened, to this extent, was probably in the 1980s, at the height of the AIDS crisis, when everyone remembers the great work the NCI did for that public health crisis. So, it is unusual for the NCI to be asked to take on something like this, but it is not unheard of. And these are very unusual times for the National Cancer Institute.
Therefore, we are eager to use these funds in the manner Congress intended with the help of NIAID to fund the best of serologic science conceivable, which will be a benefit for all Americans, including Americans with cancer.


Lastly, on the supplemental funding, we envisioned spending these monies in three buckets. The dollar amounts are still being worked out, and there’s still a lot of planning to go here. But we have been asked strongly by Congress and other parts of government to support the building of capacity, to help develop, largely, we think, academic institutions to be able to take on more serology testing, and also to be going to use those results for interesting types of clinical trials, like seroprotection studies and convalescent serum studies.
And that’s the top bucket there. And then, also, we envision using some funding for clinical serological sciences, which are larger clinical trials. And things like the COVID and Cancer Consortium and the clinical trial Jim Doroshow spoke about last time, about doing COVID-19 outcomes in patients with cancer and NCORP network, and then, also, more classical serological surveys and seroprotection studies.
Then, the last bucket, the blue bucket is really funding for foundational serological sciences research. And that would create serological sciences and centers of excellence that would do more basic immunologic research related to serology and other parts of the immune system.
Singer on serology research program:
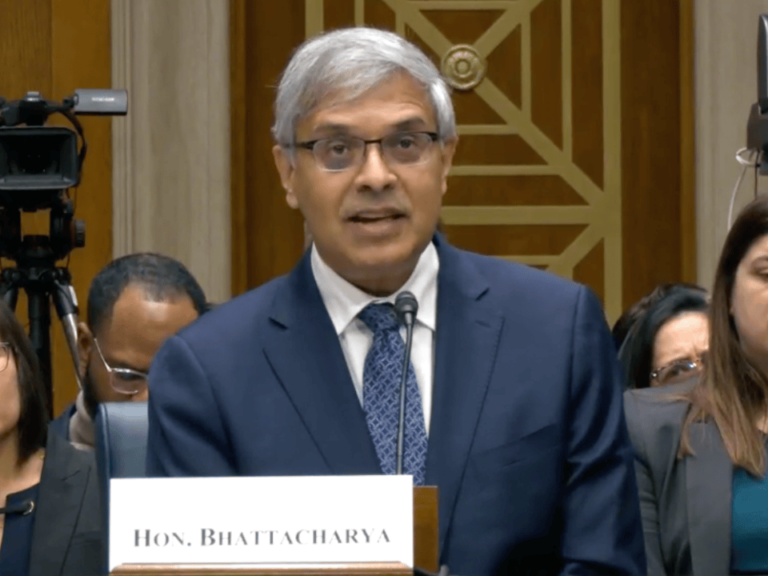
Singer: Ned started off the meeting by saying how almost the entire day was going to be focused on NCI’s plans to advance cancer research. I’m going to end the day by transitioning to talking about COVID-19 and bring you up to date on what’s happened in NCI’s COVID-19 activities, since we met just last month.
In particular, I’m going to be focusing on our current plans for a Serological Sciences Network. Ned showed you this slide in his talk in which he mentioned that on April 24, Congress passed the Paycheck Protection Program and Health Care Enhancement Act.
In that bill, NCI was directed to develop, validate, improve, and implement serological testing and associated technologies. To that end, Congress appropriated an additional $306 million on top of NCI’s FY 2020 budget.
I’ll reemphasize the point that Ned made that these funds are separate from and do not affect the RPG pool or any of the concepts that you’ve heard about today. The goal of the bill is to urgently increase the serological testing capacity and our understanding of the immune response to the SARS-CoV-2 infection. As a result, we tried to move very quickly to respond, and intend to use an emergency authorization, to implement the overall plans that I’ll be presenting to you today.
To rapidly support the expansion of serological testing capacity and expanded research on the effort from the effects of SARS-CoV-2 viral infection, we’re proposing a Serological Sciences Network, which we’ve tried to illustrate in this slide, to give you an overall view of what we are proposing.


The network is intended to work collaboratively to expand national testing capacity as quickly as possible, to develop novel serological assays, and to enhance our understanding of the viral infection, and of the immune response to that viral infection.
The network, as we planned it, will consist of five components.
First, the HPV Serology Lab at the Frederick National Lab, The lab is going to focus on validating serological tests for the SARS-CoV-2.
Next will be Serological Capacity Building Centers that will either acquire or develop and validate serological tests and, importantly, implement the testing.
We’re also planning Serological Centers of Excellence, as well as individual projects, which are going to pursue research programs in serological science.
Finally, a Coordinating Center, which is the turquoise oval in the center, which will coordinate all of these activities.
The network, I should point out, is being developed in close collaboration with our colleagues and NIAID, which has participated in the development of the plan, to ensure that it complements and enhances the efforts that that institute is currently undertaking.
We plan to have them continue as collaborators in this network. In the remaining slides, I’m going to just briefly describe each of these components.
Starting with the FNL Serology Lab—that’s going to be at the core of the network. At the last board meeting, Doug [Lowy] told you about the work that that lab is already doing, in partnership with FDA, to develop validation panels and validate serological testing and assays. [This] is an integral part of the network.


We expect the Serology Lab will continue to implement and qualify ELISA assays for IgM, IgG and we hope, IgA. It’s going to acquire and characterize serum samples from patients and controls.
The patient samples will come from people at various stages of disease, with varying titers of the antibodies. The controls are going to include serum from individuals, which were acquired prior to last September, and from individuals known to have flu and other coronaviruses, to be able to detect cross-reactivity, and also from HIV-positive individuals.
The samples that the lab acquires are going to be used to establish and, importantly, disseminate panels for validation by serological and other immune-relevant assays. Importantly, the lab is going to develop and disseminate assay standards for the entire community.
As effective as the Serology Lab has been, and we are certain, will continue to be, we also realize it can’t meet the critical needs for testing by itself. So, the Capacity Building Centers that we’re proposing are intended to extend the efforts of the Serology Lab and to collaborate with it.
The goals of these centers would be to develop and expand testing capacity across the country. To do this, the centers will be expected to either acquire already validated assays, or to develop and validate novel assays and submit them to the FDA for EUA approval. Using these set assays, the centers will be expected to deploy them to screen about 10,000 sera per week.
We’re also going to require the centers to acquire convalescent serum for possible therapeutic use, and also to conduct surveillance trials in recovered patients.
They’ll also be able to pursue some limited studies in serological sciences, using the acquired serum.
We’re proposing to support the centers through contracts to academic or private sector organizations. We anticipate that we’ll be funding between four to eight contracts at about $3 million per year for up to four years, depending on the national needs for testing. We’d like to implement these contracts to be as flexible as possible to be able to respond to the current needs and focus their efforts appropriately.


The efforts of the Capacity Building Centers, which are contracts, and the Serology Lab at FNL, we would like to complement by a series of Serological Sciences Centers of Excellence. These centers really will be focused on basic questions of science, on understanding the mechanisms that drive the serological humoral and cellular immune responses to this virus, and to determine the serological correlates with disease, pathogenesis and protection against future infection.
So, the goals of the centers broadly writ would be to characterize the immune response to the virus and the mechanisms underlying that response, to determine the serological correlates with disease, pathogenesis, and protection, to address issues related to access and co-morbidities, as well as improved population-based models, outbreak and susceptibility.
I’ll also note, relatively little is known about the immune response to SARS-CoV-2 in people with pre-cancers, those undergoing therapy, who have cancer, or cancer survivors.
We don’t know whether the susceptibility to infection or disease progression is tumor type-specific. And so, for a lot of reasons, we’re also planning to give preference to applications that include a component that is focused on the relationship of COVID and cancer.
We’re planning to use a U54 centers mechanism for these Centers of Excellence, where each center would be expected to have two to three projects that address significant questions in the immune response to COVID-19, an administrative core, and the option of a technical core, with an anticipated budget of up to $2 million per year, for up to five years.


Included in that budget, we’re going to have a set-aside of 10% to support collaborative projects across the entire network.
Again, to try to allow maximum flexibility in this very rapidly changing period, these are going to be phased awards, with an initial two years of funding, followed by the possibility of up to three years of funding, but that will give us an opportunity to pivot within these centers as necessary. We expect to make these awards by September of this year, with a very rapid turnaround.
We recognize that while some groups are going to be in a position to quickly assemble a center with all of the components that we’re asking for, we also know that there are going to be other groups who have meritorious proposals, but don’t have the time or the resources to apply for a centers grant.
So, we’d like to also support individual projects whose goals would be parallel to those of the U54, but not require the organization of a center. These projects would be funded through the U01 mechanism, with budgets of up to about $500,000 per year for up to five years.


Like with the U54s, we put the 10% set-aside for collaborative projects, again, to work across the network. Again, these would be phased awards, to give us maximum flexibility to respond to the needs as they evolve. We would hope to fund between five and 10 of these.
What we would like to do is to publish both of the RFAs for the U54s and the U01s, using the emergency FOA authorization, and publish them in the beginning of June, with a response time of about one month to six weeks. To allow investigators a little bit more time to think about.preparing these applications, we’re also planning to issue a notice of intent to publish as soon as possible—and as soon as the BSA concurs.
In everything I’ve laid out here, the fundamental assumption is that within the network structure there’s going to be a close and ongoing interaction among all of the components.
We expect a rapid sharing of serum samples of resources and data and knowledge, and cross comparison of results, and a coordination of efforts.
The success of the network is going to really depend on our ability to effectively integrate across all of those components. Therefore, we’d also like to propose to establish a Coordinating Center ,at the Frederick National Lab, that would be responsible for program management, coordination and communication across the network, sharing the data, reagent, samples and assays, and, hopefully, also to facilitate partnerships with other organizations.


I should emphasize that in all of this, or we expect the Coordinating Center to work very closely with program staff. The Coordinating Center would be established through a task order with the Frederick National Lab. We haven’t settled on an exact budget for that, we figure it will be around a 750K total costs per year. Again, with flexibility, depending on the needs at the time.
Planning for this network has moved very quickly, and we’re fully aware that we need input from the broader research community on what are the critical scientific questions and the scope of science to be supported through this network.
Therefore, we’re planning to publish a Request for Information. That RFI is going to be open for 10 days for responses, which would be reviewed by NCI program staff and incorporated into the design of the network. Leaving it open for only 10 days isn’t optimal, but necessary in order to stay within the time frame that we were required to work.


To summarize, we’re planning to establish an integrated network of cores and centers that will collaborate to advance our national capacity for serological testing as well as our understanding of the immune response to SARS-CoV-2. I’ll remind you that the legislation that directed NCI to develop and implement this program was passed just two weeks ago.
We’ll continue to flesh out the specifics as we hear feedback from you today and from the RFI, but given the very tight timeframe that we’re working in, we’d really like to ask for BSA concurrence to proceed with the two RFAs for the U54 centers and the U01 projects.
I’d like to close by saying how very grateful I am to the many people who’ve been working nonstop to make it possible for me to make this presentation today. I really sincerely thank the NCI staff listed here and our NIAID colleagues, all of whom worked tirelessly, participating in the discussions and planning that led to this network concept. With that, I’m happy to answer questions.
Dafna Bar-Sagi [BSA chair, the Saul J. Farber Professor, Department of Biochemistry and Molecular Biology, executive vice president and vice dean for science, and chief scientific officer NYU Langone Health New York University School of Medicine]: Thank you so much, Dinah. We all understand how much effort is involved in putting those together with such a short turnaround time. Great, great work from you and the entire staff. Any questions that someone have here for Dina?
Maybe I will start, Dinah, by asking you… There was one thing that I didn’t see there, but I’m not sure whether it was just an omission, not necessarily intentionally not there, which is, some interface with samples from clinical trials and how serological tests, or serology in general, is going to be potentially helpful for interpreting results from clinical trials. Is this something that you would be entertaining?
You talked a lot about the testing and things of this nature. I just wanted to get your thoughts about it, because I think there is potentially very important information there.
Singer: Right. This is something that we’ve actually been talking about, and talked about as early as this morning. I don’t know, Ned, if you want to comment on that, on the extent to which the serology lab is going to be working to do that.
Sharpless: I think getting access to materials is a really important part of this. The serology lab at Frederick needs material. In fact, many of you or your cancer center directors, I contacted about sharing samples, and I really appreciate the support we’ve gotten from the cancer centers. It’s been very, very helpful, but you know, one of the parts of the Capacity Building Centers is to do research in convalescent serum. That also has the happy byproduct of producing large volume samples that we could use for, say, creating performance panels that we could distribute to labs across the country.
Doug [Lowy, NCI principal deputy director], if he’s on, may also have thoughts on this. Doug has been largely directing the Frederick National Lab serology efforts and has thought deeply about the needs, the issues and its role in coordinating among the various mechanisms Dinah described. In any event, the faster networks would be the Capacity Building Centers, that would be a quicker mechanism through contracts, and they should be supplying samples. We also expect they will do some limited research related to serum protection and serum surveillance, but those more researchy questions will take longer, with the awarding of the RFA.
Keith T. Flaherty [director for clinical research, Massachusetts General Hospital Cancer Center]: So, Dinah, this is an exceptional start, and I can only applaud the effort with which it has been put together. I wonder if it’s outside of the scope of this mechanism… I’m wondering what the handoff is, to Ned’s point, if I’m going to go to convalescent plasma research, but also neutralizing antibody therapeutic development. There’s a very natural pass-off, as you’re well aware, between those antibody responses that are truly neutralizing, and how that would inform a convalescent plasma or engineering of off-the-shelf antibody therapeutics. And so, if that’s outside the domain, that’s totally understandable. I’m wondering what the handshake is between this program and those efforts. And if not in year one, then when.
Singer: That question, along with the question of the antibody dependent enhancement ones that could be components of the U54. Although I think for the neutralizing antibody, the challenge will be to get either viral particles or viruses that could be used to figure out whether they’re neutralizing antibodies, I think we still need to discuss it. It’s sort of borderline. Clearly, it’s an important issue.
Sharpless: I would say, we are well integrated with a therapeutics push related to coronavirus. That’s this program called ACTIV that Francis Collins is directing. We do envision neutralization assays as being part of this proposal. So, there is a BSL-3 facility at Frederick National Lab, the neutralization assays, and we also fully expect some of the fundees that would come in on either the contract mechanism or the RFA will have neutralization assay capacity as well.
And then we’re hoping people invent sort of more high throughput screening approaches that don’t require a BSL-3 facility. That would be a research question we would be eager to fund. We think what we would learn from that would then be handed off to the monoclonal antibody people who make therapeutics. But the actual trial, just the passive trial of convalescent serum could happen within some of these centers, for example.
I, for one, will be very surprised and very sad if we don’t get some new cancer antibody work out of this, because it’s just so natural.
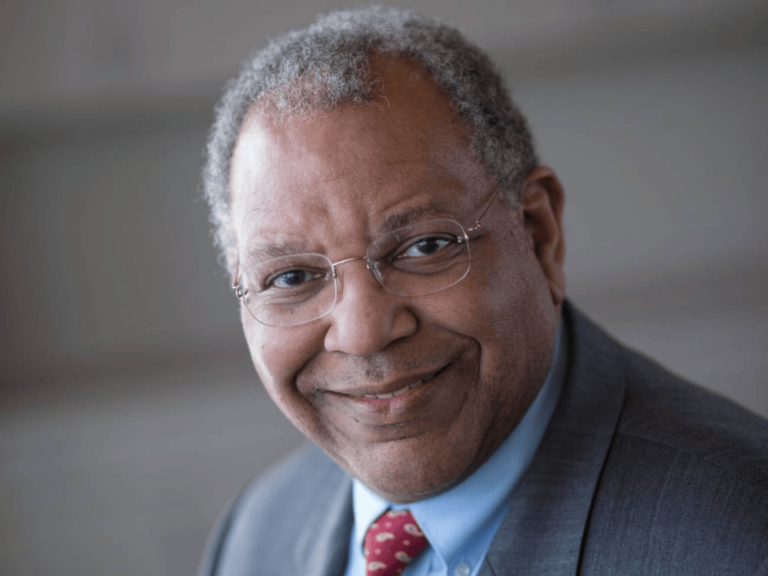
Ned Sharpless
David A. Tuveson [The Roy J. Zuckerberg Professor, director of the Cancer Center, Cold Spring Harbor Laboratory]: It seems like this topic is one that would be perfect also for a cancer center addendum. Probably half of all cancer centers think or work on this topic, I guess. Maybe more. And you could seed-fund it, and then just pick your winners from the 70 cancer centers to do a bigger project in years two [on], you’re trying to phase it. Let everyone run, and modest amount of investment, just see who actually can deliver in a year, and then you have your natural partners to move forward.
Singer: Yes, Dave, as you know, we did go out to the cancer centers, with a call for ideas on COVID-19. As a result of that, we are funding a collaboration on serology that will examine some of these questions. But I think for what we’re looking for in terms of serological sciences, that we really want to have a broader sweep of what’s out there in the community, to bring in the virologists and the immunologist who may not necessarily be in cancer centers now.
Robert D. Schreiber [The Andrew M. and Jane M. Bursky Distinguished Professor Director, Center for Human Immunology and Immunotherapy Programs, Department of Pathology and Immunology, Washington University School of Medicine]: Dinah, I also want to congratulate you there. That was just spectacular. And in such a short period of time, maybe you can come over and help me write my grant.
The other thing that is just tailor-made for us, as the NCI, is the fact that we collect longitudinal samples on our patients as we monitor them. And so, there’s probably goldmine sitting there, in the old ones, as well as the newer samples from patients that have gone through some of these infections, perhaps.
Especially, we don’t know how many have been walking around with the infection anyway. So, I do think it’s a great idea.
One thing against Dave’s idea of cancer center is, this is a perfect opportunity for us as cancer immunologists, cancer biologists, to interact with our colleagues who are the microbiologists, and many of our institutions have these parallel efforts going between the different groups. This could be the thing that brings everybody together. So, I really think this is a great idea.
Sharpless: Bob, let me say, I, for one, will be very surprised and very sad if we don’t get some new cancer antibody work out of this, because it’s just so natural, and I agree exactly with what you said.
To rapidly support the expansion of serological testing capacity and expanded research on the effort from the effects of SARS-CoV-2 viral infection, we’re proposing a Serological Sciences Network.
Dinah Singer
Cheryl L. Willman [The Maurice and Marguerite Liberman Distinguished Endowed Chair in Cancer Research, UNM Distinguished Professor of Pathology, UNM School of Medicine Director and CEO, University of New Mexico Comprehensive Cancer Center]: I really agree with you, Ned. And Bob, I agree with your comments too. Just a quick question about the mechanism. First of all, Dinah, fantastic as always, and obviously you haven’t been sleeping much. That’s a lot of work since our call a few weeks ago. But does the funding mechanism allow for consortia between academic entities, immunologists, microbiologists, pathologists, and large reference laboratory systems, which would likely hold gazillions of samples?
Singer: What I didn’t mention, and I should have, was that we would hope that some of the U54 centers will actually have private sector components, because I think that will enrich it and will increase the ability to get enough samples. We’re also going to look into the possibility of having SBIR grants to bring in some small companies. So, we’re exploring all those options. I just didn’t have time to go through all of them in a short presentation.
Willman: In the West, we have large academic-affiliated reference labs that cover pretty vast regions. So that would be really useful, if that was allowed.