Throughout Jim Allison’s early career, the field of oncology appeared to be unfazed by his T cell research.
Allison’s introduction to the now-famed immune cell came in an undergraduate immunology course, where even the professor was apprehensive about Allison’s fascination with the recently discovered T cells.
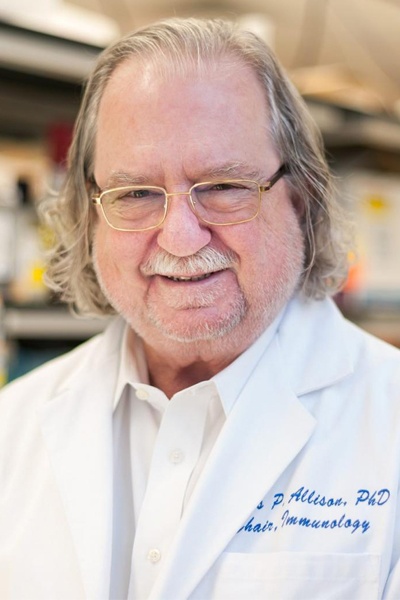
“I remember going to see the professor after class and asked, ‘Well how does that work? How do they recognize that something is wrong?’” Allison, a Nobel laureate whose research led to the discovery of the T-cell antigen receptor and the anti CTLA-4 antibody ipilimumab, and director of James P. Allison Institute, Regental Chair of Immunology, and vice president of immunobiology at MD Anderson Cancer Center, said to The Cancer Letter. Allison is also the Olga Keith Wiess Distinguished University Chair for Cancer Research and executive director of the Immunotherapy Platform.
“And he said, ‘Well, nobody knows.’ He didn’t even think there was such a thing as T cells, because he was an antibody guy, through and through. He just thought it was some kind of weird macrophage that picked up an antibody molecule.”
Allison was not convinced. He wanted to understand how these cells worked.
“At the time, the T cell receptor hadn’t been discovered. The thing that T cells use to recognize things had not been discovered. I mean, there was a lot in the literature, but it was all over the place and confusing, with a variety of different structures, and not particularly informative from what I could tell,” Allison said. “So, I set out to do that, and ended up working out the structure of the T cell antigen receptor.”
He continued to work with T cells, but his transition from fundamental immunologist to Nobel Prize-winning tumor immunologist came from the discovery of CTLA-4’s therapeutic potential.
Allison and his team had been doing research with CD28, a co-stimulatory molecule that he describes as the “gas pedal” of the immune response. He became interested in a highly homologous molecule, CTLA-4, which others in the field believed to be another “gas pedal” molecule.
There’s never been a better time to be in biomedical research and in cancer research. For the first time, we can use the words cure and cancer in the same sentence—for a fraction of patients, to be sure—but it’s beginning to be within reach.
Allison’s experiments showed, however, that CTLA-4 was actually a “brake” to stop immune responses. With this discovery, the pieces began to fall into place.
“By then we’d done a lot of experiments in the lab, showing solid tumors were invisible to the immune system,” Allison said. “It occurred to me that, maybe because of that, the tumor got a head start. The immune system was late to catch up.
“Unlike viruses and bacteria and things that the innate immune system picks up right away—they have those second signals that say, ‘Go. This is foreign. Do something about it.’ Tumors are a little less obvious than that.”
Allison and his team quickly began doing experiments on CTLA-4. All they had to do was inject antibodies to CTLA-4, and “the tumors just melted away.”
Despite the experiment’s success, Allison’s colleagues were not enthusiastic.
“We presented the data at the International Congress of Immunologists in San Francisco in 1995 and it was greeted by a very wide and mediocre yawn by most of the science community. ‘Oh yeah, somebody else curing tumors in mice.’”
It was a matter of bad timing.
“Unfortunately, the world of cancer therapy had sort of passed through the immunology phase that was popular in the 60s and 70s,” Allison said. “There had been so many failed trials, particularly with vaccines, that people began to think tumor immunology was strictly a property of mouse models and would never work in humans. The net result was me shouting into an empty room most of the time for years.”
Allison trusted his data, and it led to a novel treatment that is life-altering for many.
“Data speaks to you. Design an experiment right, you’ll get a good answer, but you’re never going to get a perfect answer.”
The important thing is to stay open-minded, Allison said.
“No scientists should ever say the words, ‘It never works or it never will.’ I mean, that’s what a scientist is about; right? Moving forward, making things, finding out something new—where you can make something happen that never had before,” Allison said.