A year after starting his job as NCI director, Ned Sharpless is reviewing the entire spectrum of NCI research in an effort to focus on areas where the institute plays a key role.
NCI is able to make these decisions in fiscal 2019 more efficiently, because for the first time in two decades, the spending bills have cleared Congress on time (The Cancer Letter, Sept. 28).
Managing expectations is one of the problems Sharpless faces at a time of increasing funding.
“Because the majority of NCI grants are for multi-year research efforts, our grant portfolio includes multi-year commitments,” Sharpless said to The Cancer Letter, responding to a question about his plans for stamping his vision on the institute.
Sharpless said that even though NCI has received a $400 million bolus of Moonshot funding, which will drop to $195 million in fiscal 2020, the institute may end up reserving some for the new funds for a smooth downward transition. “The funds provided by the 21st Century Cures Act are not constrained by fiscal year, so they can be spent with greater flexibility than other funds in the general appropriation,” Sharpless said.
In a conversation with The Cancer Letter, Sharpless said he has convened working groups to help him prioritize the institute’s programs.
“We can all agree that additional funding authorized by the Cures Act is good news, but the road ahead is far from smooth. We’re grateful to be trending upward, but we are nonetheless rather constrained. Research is expensive—increasingly so, and our grants have large outyear costs,” Sharpless said. “We must find efficiencies and we must be vigilant and strategic in our spending to ensure that the best ideas can be supported. This also means that programs that are less effective can be revisited and modified or retired.
“I am now looking at the entire portfolio—focusing on areas where NCI is an essential player, as well as areas where our role is smaller and where others should lead. I have convened working groups with extramural experts to help me and my leadership team think through our future investments.
“Obviously, the key focus areas that I have identified—basic science, big data, clinical trials, and workforce development—are areas where NCI plays a critical role. And, as you know, I increased funding for clinical trials and the RPG pool in FY 2018. I assume we will see adjustments to some areas.”
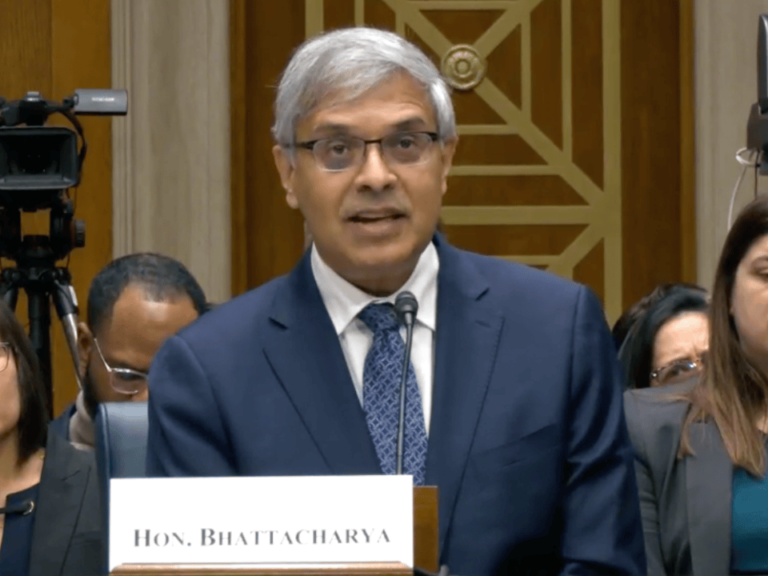
Sharpless spoke with Paul Goldberg, editor and publisher of The Cancer Letter.
Paul Goldberg: You’ve been at NCI for a bit more than a year now. How do you like the job?
Ned Sharpless: Only a year? Seems longer. In truth, I’m having a great time. It is an honor and a privilege to lead the National Cancer Institute.
Being named NCI director was not something I anticipated happening in my career, and I remain humbled to have been appointed to this position.
One thing I’ve said many times over the last year is that it is a great time to be a cancer researcher in the United States. We have a new understanding of the biology of disease, rapidly advancing technology, strong support from Congress and advocacy groups, and exciting new approaches to prevention and treatment that are helping patients.
In fact, we have never seen a period during which so many promising new therapies have become available that are providing meaningful benefits to patients. This confluence of events has generated tremendous excitement in our field. It is palpable.
And that’s a message of hope that needs to be conveyed and reinforced because I consider outreach an important component of my role as NCI director.
That’s why I spend a great deal of time in the community, speaking with and listening to stakeholders, including patients and advocates, cancer centers and grantees, other NIH and government agencies, and industry partners, as well as with NCI intramural researchers.
I’ve made it a point to learn about their priorities and challenges, and how NCI can support them. I really enjoy that direct engagement.
It has been thrilling to work with people in the NCI whose commitment to cancer science and painstaking efforts have led to groundbreaking discoveries that have resulted in steadily declining incidence and mortality rates for most cancers as well as better options for more effective, less toxic therapies.
You have a nearly $6 billion budget, not including Moonshot funding. But because of commitments to ongoing, multi-year research projects, much of that money is committed. Given these commitments, how will you stamp your vision onto the portfolio?
NS: Because the majority of NCI grants are for multi-year research efforts, our grants portfolio includes outyear commitments.
Just as I did in FY 2018, I intend to actively engage with program leaders to make sure that we’re funding the absolute best science, especially in the key focus areas that I’ve described over the last six months.
The fact that we have the 2019 budget on time, starting with the beginning of the fiscal year, makes that task much easier, and we are appreciative of the Congress and president’s work that led to a completed budget in 2019 by the start of the fiscal year.
With these extra months for planning, we will be able to identify funds to address these new priority areas.
To what do you attribute NIH and NCI’s recent good fortune in the appropriations process?
NS: Cancer is a bipartisan issue and our continued progress in advancing the field can’t be denied.
Congress is very interested in NIH. I’ve had more interaction with members of Congress than I expected at this point in my tenure, which says a lot.
I have been impressed with the level of understanding of cancer research by both members of Congress and their staff. Their response has been very positive. Not only do they hold hearings and briefings, but they also visit the NCI.
They meet with our researchers—intramural and extramural—and with our patients. They engage in really meaningful ways. You can tell they learn a lot, and they express a lot of enthusiasm and support for our work.
I also have to say that the cancer research community—both scientists and patient advocates—do a terrific job with engaging with Congress and grounding discussions about appropriation numbers in terms of the patient experience, highlighting both hopes and challenges of the opportunities ahead.
Let’s focus on the Moonshot. This year’s Moonshot funding is at the highest level—$400 million, up from last year’s $300 million. But then, next year, comes a drop—to $195 million. How will you spend the money you have this year in a way that will make a difference? And how will you plan for next year’s drop-off?
NS: The 21st Century Cures Act authorized seven years of funding for the Cancer Moonshot and NCI has been planning for this funding fluctuation since the bill was signed into law.
The funds provided by 21st Century Cures are not constrained by fiscal year, so they can be spent with greater flexibility than other funds in the general appropriation.
We are continuing to expand our Cancer Moonshot portfolio in FY 2019, including planning for implementation of longer-term scientific initiatives.
Okay, let’s move away from the Moonshot. In NCI’s regular appropriations, are there programs that will get more money? Are there programs that, in your opinion, have enough and don’t need any more? Programs that get more than they should? Let me just rattle off a few programs: R01 grants, cancer centers, SPOREs, NCTN, NCORP, the intramural program, Frederick.
NS: As mentioned, NCI is very pleased to have our first on-time appropriation in more than 20 years. We’re actively working to make decisions about FY 2019.
We can all agree that additional funding authorized by the Cures Act is good news, but the road ahead is far from smooth.
We’re grateful to be trending upward, but we are nonetheless rather constrained.
Research is expensive—increasingly so, and our grants have large outyear costs. We must find efficiencies, and we must be vigilant and strategic in our spending to ensure that the best ideas can be supported. This also means that programs that are less effective can be revisited and modified or retired.
I am now looking at the entire portfolio—focusing on areas where NCI is an essential player, as well as areas where our role is smaller and where others should lead.
I have convened working groups with extramural experts to help me and my leadership team think through our future investments.
Obviously, the key focus areas that I have identified—basic science, big data, clinical trials, and workforce development—are areas where NCI plays a critical role. And, as you know, I increased funding for clinical trials and the RPG pool in FY 2018. I assume we will see adjustments to some areas.
People in the extramural world used to look askance at the intramural program. It looks to me at least that they have been proven wrong. This doesn’t look like a question, but it is.
NS: Yes, they have been proven wrong. Over the last year, I have become even more steadfast in my belief that NCI’s intramural research program is very strong and critical to advancing cancer research.
The intramural program allows researchers a lot of freedom to do science, and to work in teams on highly basic problems to highly translational efforts.
Undeniably, the intramural program has produced paradigm-changing research, as you know because you’ve covered our work in The Cancer Letter. Just to name a few examples… the work of Doug Lowy and John Schiller in developing HPV vaccines—one of the most important cancer prevention discoveries in the last century; Steven Rosenberg’s team and their groundbreaking work to develop immunotherapies and gene therapies—now considered a fourth modality for treating cancer; Lou Staudt’s definitive work in cancer genetics and lymphoma; Brigitte Widemann’s work towards developing a first therapy for neurofibromatosis; Andre Nussenzweig’s pioneering studies in DNA metabolism and replication; Marston Linehan’s pivotal studies of the genetic basis of kidney cancer; and fairly recently, FDA approval of moxetumomab for hairy cell leukemia—initially discovered by Ira Pastan’s group, and then advanced through collaboration with a pharmaceutical partner. Ira has been a long-term leader in the development of antibody-drug conjugates and this FDA approval is an immense achievement.
And that’s just NCI’s Center for Cancer Research. In our intramural Division of Cancer Epidemiology and Genetics, our researchers have been uniquely positioned to conduct long-term studies of occupationally-exposed populations as well as other special populations.
Using data from nine historical cohort studies, DCEG’s Mark Little, Amy Berrington de González, Martha Linet, and their collaborators were able to quantify—for the first time—excess risk for leukemia and other myeloid malignancies following low-dose exposure to ionizing radiation in childhood. Another DCEG team including Nicolas Wentzensen and Megan Clarke led a prospective study demonstrating a new test can help to improve the clinical management of women who screen positive for HPV infection in routine cervical cancer screening.
The OncoArray Network is a fantastic example of intramural-extramural collaboration. Through this consortium, DCEG researchers collaborate with grantees funded through NCI’s Division of Cancer Control and Population Sciences to gain new insight into the genetic architecture and mechanisms underlying common cancers. This international team of scientists recently identified 63 new genetic variants associated with risk for prostate cancer. Results from this study may help improve the identification of men at high risk for prostate cancer and inform PSA guidelines for screening and management to reduce the burden of over-testing.
All of these examples—and so many more—have demonstrated for me that the NCI intramural program is full of energized, world-class scientists pursuing challenging and rewarding investigations across the spectrum of cancer research—basic, clinical, epidemiological, and population sciences.
What about Big Data? Is it in any particular spot, or is it everywhere, like God and germs?
NS: Let’s face it, we live in an era where information is being collected in a wide range of contexts about every aspect of our lives.
We live in a sea of big data and we will drown in it if we don’t learn to swim. To do that, we have to intentionally standardize our collection and aggregation processes and analyze the vast amounts of data with the proper tools and computational approaches. In the case of cancer research, big data holds a great deal of power to unlock the mysteries of understanding and treating cancer.
By aggregating different types of data from large samples of patients—for example, linking genomic, pathology, radiology, and clinical data mined by machine learning—critical relationships between cancer type and treatment that otherwise would not emerge from traditional analyses may become obvious.
Such efforts would allow us to learn from every patient’s data, improve our understanding of cancer, and make better treatment decisions. In more ways than I can count, we owe that progress to our patients, and NCI can play a much-needed leadership role in helping us get from where we are today with big data to where we need to be.
Could we talk about the Bypass Budget? We don’t talk about it often enough. How does your Bypass Budget differ from Bypass Budgets past?
NS: This critical tool is something I learned about early in my tenure and, like my predecessors, I see the plan as an opportunity unique to the NCI director that allows the institute to submit a cancer research request outside of the normal federal budget process.
I’m happy with the way the FY 2020 Annual Plan & Budget Proposal bridges the key focus areas that I rolled out this past spring, and they are clearly woven throughout each chapter.
My hope is that readers will find this plan to be more focused on the impact of NCI’s work on patients, including one of my own. I’ve always said that patients are our true partners in cancer research and the reason we do what we do.
What are you hearing from young investigators? Have the recent budget increases rescued what Francis Collins used to worry as a “lost generation?” What are your thoughts about proposals to shift more funding toward first-time investigators?
NS: There’s no question that training the next generation of cancer researchers and supporting them as they begin their careers as principal investigators is essential to making progress for cancer patients and their families. This is both an institutional priority for NCI and a personal priority for me.
We are unwavering in our goal to fund the best cancer research and the PIs who conduct it at all career stages.
Research is expensive— increasingly so, and our grants have large outyear costs. We must find efficiencies, and we must be vigilant and strategic in our spending to ensure that the best ideas can be supported.
There are issues particular to early-stage investigators. For example, one challenge for early career investigators is entry into the R01 funded workforce due to low pay lines and increased competition. NCI committed to funding at least 25 percent more ESI in FY18 compared to the prior fiscal year. Not only did we achieve this goal, but we surpassed it.
Another challenge for ESIs, is once they have entered the workforce, they need to sustain a vibrant career by attaining their next substantial NIH award.
We are piloting an ESI MERIT Award program initiated in FY18. This program awards an R37 grant to highly meritorious applications submitted by ESIs for up to 7 years instead of the traditional 5-year period.
The intended goal is to provide addition time to the awardees to prepare a second competitive application, to reduce stress and administrative burden, and increase the opportunity for conducting high-risk and innovate research. NCI funded more than 60 ESI MERIT Awards in FY18 and looks forward to continuing this pilot into FY19.
What’s the biggest difference between leading a cancer center and leading NCI? What’s got you most jazzed about leading NCI, compared to a cancer center? Have you encountered any roadblocks that you hadn’t anticipated? Let me put it another way: what should your former extramural colleagues understand about how NCI works?
NS: I know firsthand the priorities and challenges of running a cancer center, and in my role as NCI director, I’m planning to actively work with cancer centers to mitigate their challenges.
Take for example, the need for reduction of operational burden. I have increased per-patient reimbursement for enrollment in NCI-sponsored clinical trials, something cancer centers play a critical role in, so that accrual costs are more competitive with industry-sponsored trials.
NCI is committed to having patients enrolled in the best trials to advance patient care regardless of trial cost. We are also looking at possible ways to reduce the administrative burden of applying for Cancer Center Support Grants. And, because the NCI Cancer Centers Program is one of the anchors of the nation’s cancer research effort, we are hoping to expand the number of centers across the country as resources allow.
Of course, I believe that listening and learning is an important component of my role as director of the national cancer program, and I visit cancer centers regularly to keep our dialogue ongoing so that NCI can support them to do the best science possible.
Anything else? What haven’t I asked?
NS: As mentioned, our progress in cancer is rapid at present.
I think one challenge this good news presents is that we’ve almost become inured to the fact that we have been seeing and will likely continue to see remarkable findings reported at the scientific meetings each year—the kind of results that we would have been over the moon about ten or fifteen years ago.
It’s become the new normal and that’s great for the patients we serve. I’m thrilled to be leading the NCI at this exciting and important time.